Thursday, June 30, 2005
Dr. Parker's Game Reviews: SWAT 4......
A very well-done first-person tactical shooter. You lead a squad of four through 13 missions involving hostage rescue and "high risk warrant service" You get extra points for arresting the bad guys rather than killing them off. You have a wide choice of lethal and "less lethal" weapons to accomplish this goal. The team AI is pretty good. That is if an unauthorized force penalty is assessed, it will probably be you that causes it to occur.
The game is easily replayable, as the bad guys and hostages appear in new locations after each mission is played.
Multiplayer also available. |
A very well-done first-person tactical shooter. You lead a squad of four through 13 missions involving hostage rescue and "high risk warrant service" You get extra points for arresting the bad guys rather than killing them off. You have a wide choice of lethal and "less lethal" weapons to accomplish this goal. The team AI is pretty good. That is if an unauthorized force penalty is assessed, it will probably be you that causes it to occur.
The game is easily replayable, as the bad guys and hostages appear in new locations after each mission is played.
Multiplayer also available. |
Wednesday, June 29, 2005
Do You Know Where that Finger has Been??????
A follow-up to this post. The one that had this picture:

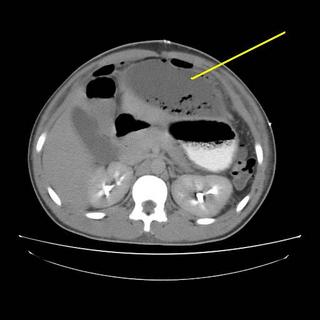
The patient progressed slowly with low-grade fevers and leukocytosis. He had persistent free air as well so after a few days I obtained a CT Scan:
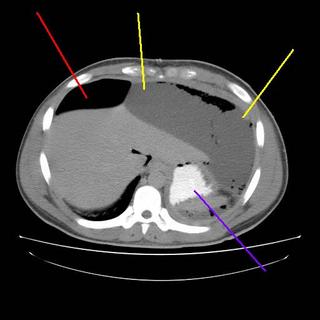
The yellow lines are a subphrenic fluid collection, likely an abscess. The red line is more free air and the blue line is contrast in the stomach. Interventional radiology again saves the day with a pigtail catheter.
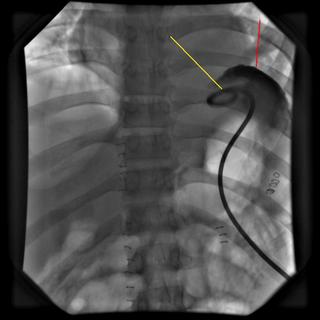
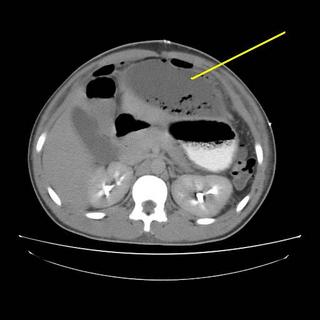
The yellow line points to the catheter, red demonstrates contrast within the cavity. About 1500cc are removed initially with decrease in WBC and the patient becomes afebrile. A repeat scan is obtained a few days later:
The patient had received 24 hours of Ancef postop. The cultures grew out S.viridans so a missed visceral injury is unlikely. He was taking a regular diet throughout the above events. He was discharged a day after the repeat CT. I saw him recently in the office and he is doing well. |
A follow-up to this post. The one that had this picture:

The patient progressed slowly with low-grade fevers and leukocytosis. He had persistent free air as well so after a few days I obtained a CT Scan:
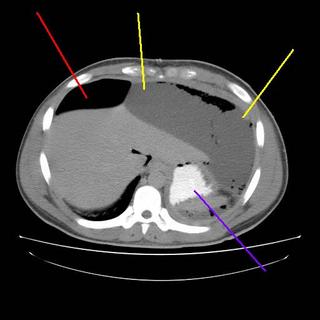
The yellow lines are a subphrenic fluid collection, likely an abscess. The red line is more free air and the blue line is contrast in the stomach. Interventional radiology again saves the day with a pigtail catheter.
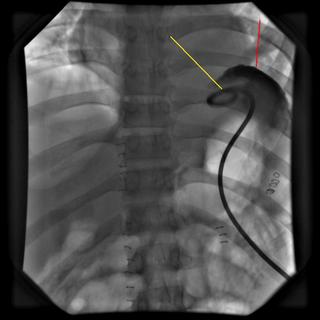
The yellow line points to the catheter, red demonstrates contrast within the cavity. About 1500cc are removed initially with decrease in WBC and the patient becomes afebrile. A repeat scan is obtained a few days later:

The patient had received 24 hours of Ancef postop. The cultures grew out S.viridans so a missed visceral injury is unlikely. He was taking a regular diet throughout the above events. He was discharged a day after the repeat CT. I saw him recently in the office and he is doing well. |
Tuesday, June 28, 2005
Thursday, June 23, 2005
The Search for Laparotomus Rex....
Aggravated Doc Surg has an excellent analysis (included in what even I have come to realize was an overly-long Grand Rounds) of an editorial in the June issue of the Journal of the American College of Surgeons($):Enough, but Not Too Much: Or, Are We the Dinosaurs? Laparoscopy has almost taken over:
My take: Laparoscopic cholecystectomy has a well-proven track record of safety. It has advantages of reduced pain, reduced stay in hospital, and earlier return to activity.
In my hands my open appendectomy patients are discharged the next day, have good pain control, and return to normal activity (excluding heavy labor) in a few days. I myself cannot justify the added expense of the laparoscopic procedure given the results. YMMV, however. Further thoughts here.
I reserve laparoscopic inguinal hernia repairs for recurrent hernias (the anatomy is less distorted) and for bilateral hernias (pain control). Otherwise I perform a "plug-and patch" via an open anterior approach.
Laparoscopic ventral hernia repair allows for full visualization of defects. Useful in the "swiss cheese" scenario of several small defects. Recurrence rate is reduced, but LOS/pain control about the same between the procedures.
Still on the learning curve for laparoscopic colectomies. LOS and pain control eqivalent to the open procedure.
My partner does laparoscopic Nissen fundoplications, adrenalectomies and a few splenectomies. He is pleased with the results compared to open operations.
Neither my partners nor myself perform bariatric surgery, open or laparoscopic.
The solution? From the editorial and ADS's post:
Aggravated Doc Surg has an excellent analysis (included in what even I have come to realize was an overly-long Grand Rounds) of an editorial in the June issue of the Journal of the American College of Surgeons($):Enough, but Not Too Much: Or, Are We the Dinosaurs? Laparoscopy has almost taken over:
The effects on our training programs are as yet unknown, but the shift from open techniques to minimally invasive surgery has been tremendous. The archetypal example of the latest impact of minimally invasive surgery is the effect laparoscopic approaches have had on bariatric or obesity surgery. The American Society for Bariatric Surgery has grown in membership from 258 in 1998 to 1,070 in 2003; the number of bariatric procedures in the US has grown from 16,000 in the early 1990s to a projected 144,000 this year Laparoscopic, minimally invasive procedures have made this the fastest growing area of surgery.As my colleague points out, nobody expects to convert to open:
Although the data show that open, tension-free mesh hernias are an excellent and cheaper form of hernia repair, laparoscopic hernias are growing in popularity. In some hospitals, up to 50% of appendices are removed laparoscopically, more than 75% of gallbladders are taken out through a scope, and many diseased, nontraumatized spleens are removed minimally invasively. Laparoscopic colectomy has proved to be acceptable for cancer, and laparoscopic donor nephrectomy has become the procedure of choice for living donors.
For example, does the average surgery resident finish training with many common duct explorations? Open Nissens? Open cholecystectomies? This is not a moot point, as the "easy" cases will always be done laparoscopically --- when we convert to an open procedure, you can bet that it is because the operation is much more difficult, due to anatomy, bleeding, etcConversion is not all that rare a phenomenon:
Conversion rates for procedures vary significantly according to procedure, operator, and high-volume versus low-volume centers. Studies from several countries give a conversion rate from laparoscopic to open cholecystectomy at 9.5% to 4.8%, with an average of 5% to 10%. That means that an average chief resident will do between 5 and 10 open gallbladder procedures during residency. In a recent study from Italy, the conversion rate for appendectomy was 9.7% because of severe peritonitis or anatomy. Gastric bypass conversion is down to 3% according to a recent study. Hernias and adrenalectomy rarely need conversion, and left colectomy required conversion in 4.9%. The US randomized colon cancer trial had a 21% conversion to open rate among laparoscopic colectomies. Even perforated gastroduodenal ulcers need to be converted to an open procedure only 12.5% of the time.My program was unusual in that we had an attending that did not believe in laparoscopic cholecystectomy. He would do his through a mini-lap incision. While we all kind of laughed behind his back but we did learn how to do an open cholecystecomy. We would tell residency applicants that if they came here they would have more experience with open cholecystectomy than almost anywhere else. Looking at my submitted numbers from residency (lower than actual because I lost quite a number of the "checkbooks" we used to record cases) I either performed or served as teaching resident on 41 open procedures and 166 laparoscopic ones. I didn't finish my surgery residency that long ago,either. Only a handful of those were conversions. Moving along:
We have established learning curves for many laparoscopic and now for robotic procedures, but the question for the educators of future surgeons has to be: How many open procedures do you need to do to be safe? Ramifications of this include a revision of Residency Review Committee requirements for procedures, a revision of the oral and written boards, and a new definition for general surgery. Why do we need fellowships in advanced laparoscopy or even bariatrics if the current trend toward laparoscopic surgery continues? The attempt to pull out the cardiothoracic and vascular trainees from general surgery makes absolute sense if the majority of senior surgical residency is spent behind a camera.Sound like film school. Another argument for specialty track. The generation gap rears it's head:
So let us look at facts: The majority of the leaders in American surgery were trained in the era when minimally invasive surgery was in its infancy. The new directors and chairs are coming in at a time when the Âopen Nissen is an anachronism. How many chief residents know how to perform a common duct exploration? (Do they need to?) Giving the oral boards recently, I was amazed to find that the treatment for a strangulated inguinal hernia requiring a bowel resection was Âvicryl mesh, because very few knew what a McVay repair was. The treatment of choice for a perforated ulcer was a laparoscopic repair. The number of open gastrectomies was about equivalent to the average number of ÂWhipples performed.Nowargumentgument has more to do with the widespread use of open prosthetic hernia repair techniques than the popularity of the laparoscopic hernia repair.
How many Âopen ventral hernias does the up-and-coming resident need when he can take down adhesions with scissBobbieor bovie or harmonic scalpel) through a scope? The question becomes more important as fellowships turn out more advanced laparoscopists who will, in turn, teach residents more advanced techniques. The new generation of laparoscopic surgeons, through a combination of patience, guts, and skill, can complete the majority of operations and address complications without opening the patient. Who would have thought that you could patch a laparoscopic gastric bypass leak laparoscopically and avoid a laparotomy most of the time? What will happen to surgeons who have seen 200 laparoscopic appendices, hernias, and gastric bypasses, who realize that they canÂt do a procedure safely through a scope because of inflammation or bleeding? Will they be prepared for the open procedure?[emphasis mine]
My take: Laparoscopic cholecystectomy has a well-proven track record of safety. It has advantages of reduced pain, reduced stay in hospital, and earlier return to activity.
In my hands my open appendectomy patients are discharged the next day, have good pain control, and return to normal activity (excluding heavy labor) in a few days. I myself cannot justify the added expense of the laparoscopic procedure given the results. YMMV, however. Further thoughts here.
I reserve laparoscopic inguinal hernia repairs for recurrent hernias (the anatomy is less distorted) and for bilateral hernias (pain control). Otherwise I perform a "plug-and patch" via an open anterior approach.
Laparoscopic ventral hernia repair allows for full visualization of defects. Useful in the "swiss cheese" scenario of several small defects. Recurrence rate is reduced, but LOS/pain control about the same between the procedures.
Still on the learning curve for laparoscopic colectomies. LOS and pain control eqivalent to the open procedure.
My partner does laparoscopic Nissen fundoplications, adrenalectomies and a few splenectomies. He is pleased with the results compared to open operations.
Neither my partners nor myself perform bariatric surgery, open or laparoscopic.
The solution? From the editorial and ADS's post:
We propose that the RRC (Residency Review Committee) and the American Board of Surgery look at their requirements for essential cases and revise them to reflect the rapid rise in minimally invasive techniques. We can find no data on the number of open procedures necessary to make a competent surgeon, only total numbers. The RRC doesn't even require "advanced" laparoscopic cases. We need to talk to the young surgeons and the experts who perform primarily laparoscopic procedures, and ask what is necessary to train the general surgeon of the future. If general surgery is to survive, minimally invasive bariatric procedures, splenectomy, Nissen fundoplication, and colectomy need to be taught in residencies. We still need to teach surgeons how to do a hand-sewn anastomosis, close an incisional hernia, and take out a gallbladder through an incision, just in case there is a reason to abandon a scope and do it the old fashioned way. Oh yes, and do this in 80hours a week.Yeah, try to get that consent signed. |
In the best of all possible worlds, newly minted surgeons would take jobs with older, more established surgeons that provide expertise and help ("mentoring," to use the current buzz word) -- here, again, I was and continue to be extremely fortunate in this regard. That is probably not attainable for many graduating residents. It is hard to conceive a situation where the RRC would mandate a certain percentage of cases to be done "open," either: can you imagine the consent form for patients at teaching facilities then ---- "if we determine that the resident helping with this operation has insufficient experience with the open technique, you'll get a bigger incision." That would be about as popular as Howard Dean at a NASCAR event.
Wednesday, June 22, 2005
Help from the Other Side of the Blood-Brain Barrier.....
From the Wall Street Journal, a plan to reduce liability premiums that physicians and lawyers can agree on:Once Seen as Risky, One Group Of Doctors Changes Its Ways
And saved money:
From the Wall Street Journal, a plan to reduce liability premiums that physicians and lawyers can agree on:Once Seen as Risky, One Group Of Doctors Changes Its Ways
Anesthesiologists pay less for malpractice insurance today, in constant dollars, than they did 20 years ago. That's mainly because some anesthesiologists chose a path many doctors in other specialties did not. Rather than pushing for laws that would protect them against patient lawsuits, these anesthesiologists focused on improving patient safety. Their theory: Less harm to patients would mean fewer lawsuits.They worked to improve safety and training methods, and it has both helped patients:
Over the past two decades, anesthesiologists have advocated the use of devices that alert doctors to potentially fatal problems in the operating room. They have helped develop computerized mannequins that simulate real-life surgical crises. And they have pressed for procedures that protect unconscious patients from potential carbon-monoxide poisoning.
All this has helped save lives. Over the past two decades, patient deaths due to anesthesia have declined to one death per 200,000 to 300,000 cases from one for every 5,000 cases, according to studies compiled by the Institute of Medicine, an arm of the National Academies, a leading scientific advisory body.
And saved money:
Malpractice payments involving the nation's 30,000 anesthesiologists are down, too, and anesthesiologists typically pay some of the smallest malpractice premiums around. That's a huge change from when they were considered among the riskiest doctors to insure. Nationwide, the average annual premium for anesthesiologists is less than $21,000, according to a survey by the American Society of Anesthesiologists. An obstetrician might pay 10 times that amount, Medical Liability Monitor, an industry newsletter, reports.Even the IOM likes anesthesia:
In some areas, anesthesiologists can now buy malpractice insurance for as little as $4,300 a year, although premiums ranged as high as more than $56,000, according to the ASA. The ASA survey gave no general explanation for the disparity but did note that premiums were higher for anesthesiologists who had been sued before and for those who perform higher-risk procedures.
A 1999 report by the Institute of Medicine noted that "few professional societies or groups have demonstrated a visible commitment to reducing errors in health care and improving patient safety." It identified one exception: anesthesiologistsThe watershed moment came in the early 80's:
In 1982, the ABC news program "20/20" aired a piece on anesthesia-related deaths. "It was a devastating indictment of anesthesia," recalls Ellison C. Pierce Jr., a retired professor of anesthesiology at Harvard Medical School who is considered by many to be the father of the modern anesthesia-safety movement.The process started with data collection:
Around the same time, anesthesiologists were getting hit by their second wave of big malpractice-insurance premium increases in a decade. The specialty was then considered among the riskiest to insure, and premiums were often two to three times as high as those other doctors paid. Casey Blitt, a 63-year-old Tucson, Ariz., anesthesiologist who has long been active on patient-safety issues, says his insurance soared to $50,000 a year from $20,000 or less. Dr. Pierce says anesthesiologists were "terrified," and anxious to do something.
Dr. Pierce at the time was president of the American Society of Anesthesiologists. In 1985, that group provided $100,000 to launch the Anesthesia Patient Safety Foundation. The new foundation was unusual in medicine: a stand-alone organization solely devoted to patient safety. Working closely with the larger ASA, from which it still receives about $400,000 a year, the foundation galvanized safety research and improvement.
Twenty years ago, little was known about people injured or killed during anesthesia. No U.S. database existed, so anesthesiologists set out to create one. They decided to collect information from insurers on closed malpractice claims, those in which insurers had made a payment or otherwise disposed of the complaint.The American College of Surgeons has also begun to analyze closed claims as part of the Patient Safety and Quality Initiative. They fixed big problems:
Most insurers hesitated to cooperate at first, saying they were worried about patient privacy. One company finally agreed: St. Paul Fire & Marine Insurance Co. in Minnesota said it was concerned about heavy losses it had suffered from anesthesia-related injuries and was eager for anesthesiologists to review claims. Soon, other insurers followed suit.
Anesthesiologists left their practices for days at a time to pore over closed insurance claims. The information they collected was fed into a computer at the University of Washington to create an overall picture of how anesthesia accidents tend to occur. It "was a humbling experience," recalls Russell T. Wall, an anesthesiology professor at Georgetown University School of Medicine in Washington, D.C. To date, more than 6,400 claims have been analyzed.
In part by analyzing claims, the anesthesiologists were able to document the extent to which patients were dying because of a simple mistake: Anesthesiologists were inserting the patient's breathing tube down the wrong pipe. Rather than putting it down the trachea, which leads to the lungs, they were accidentally inserting it down the esophagus, which leads to the stomach. The problem was, there was no way to determine quickly whether the tube was in the right pipe. Patients often simply turned blue or their blood turned dark. By then, it was usually too late to save them.Both of these technologies have spread far beyond anesthesia. They also solved some smaller ones:
The research contributed to two innovations that between them would all but eliminate death and injury from "intubation" errors. One, known as pulse oximetry, measures the oxygen level in the patient's blood stream by means of a device that clips onto the patient's finger. The other, capnography, measures carbon dioxide in a patient's expelled breath, which helps doctors determine at a glance that a patient is breathing properly.
That change has been accompanied by other less obvious improvements. During surgery, a patient's body temperature can fall as room-temperature intravenous fluids are infused into the blood. This cooling can cause tissue to die and make the body vulnerable to infection. The safety foundation funded research on the problem in the 1990s, and now care is taken to keep patients warm during surgery, often with specially made blankets that can be heated. Blood and fluid warmers are also used.Sometimes we as surgeons can be seen as stumbling blocks:
Anesthesiologists also have become much better at preventing patient exposure to carbon monoxide. The potentially deadly gas can be an unintended byproduct of the process of cleansing a patient's exhaled breath of carbon dioxide before the air is recycled back to the patient's lungs. One simple way to guard against this problem is to make sure that absorbent material in anesthesia machines that filters the recycled air remains moist.
In 1994, the newsletter of the anesthesiologists foundation documented cases in which patients were exposed to high levels of carbon monoxide during surgery on Mondays, presumably after absorbents had spent the weekend drying out. The organization recommended replacing the absorbent material on Monday mornings and several other changes. These are now standard practice, and rates of carbon-monoxide exposure have fallen dramatically.
Anesthesiologists are now focused on alarm bells. Modern anesthesia machines come equipped with audible alarms that sound when certain thresholds, such as oxygen levels, are crossed. But the alarms irritate many surgeons, so some anesthesiologists have turned them off. The foundation has documented 26 alarm-related malpractice claims between 1970 and 2002, or a little more than one a year. Of those, more than 20 resulted in either death or brain damage.I, for one, am not irritated by the alarms. They indicate that something is amiss. My antennae also go up if I see a bunch of movement behind the drapes. More results:
In 1972, according to a recent study by Public Citizen, a consumer-advocacy group in Washington, D.C., anesthesiologists accounted for 7.9% of all medical-malpractice claims, double the proportion of physicians who practiced anesthesiology. Between 1985 and 2001, anesthesiologists accounted for only 3.8% of all claims, roughly comparable to the percentage of doctors who were anesthesiologists.The ASA and anesthesiologists overall deserve a well-earned pat on the back for their efforts. I also applaud the ACS for the safety improvement efforts that are underway. However, I would not be surprised if the efforts by the ACS are more difficult and less successful. The improvements in anesthesia were based on solutions to problems that were, for the lack of a better word, quantifiable. Esophageal intubation is a problem, given the right tools, that can be quickly recognized and corrected. How can one quantify surgical judgment? How many variables such as experience, technique, medical co-morbidity, material, and time of day, for example; affect the outcome of surgery? Yes, safety is compromised when surgical instruments are washed in hydraulic fluid. But the biggest obstacle may be ourselves:
The size of payments from successful malpractice suits against anesthesiologists also has declined. According to the American Society of Anesthesiologists, the median payment during the 1970s was $332,280. By the 1990s, it had dropped 46%, to $179,010. These amounts are in 2005 dollars and are the most recent figures available.
Claims for serious injuries have become less frequent. In the 1970s, according to the ASA, more than half of anesthesia-malpractice claims involved death or permanent brain injury. In the 1990s, that fell to less than one-third of claims.
Malpractice rates for anesthesiologists have gradually fallen, the ASA says. This year, the average annual premium is $20,572, compared with $32,620 in inflation-adjusted dollars in 1985. That's a decrease of 37% over 20 years. Malpractice rates are generally set at the beginning of the year.
At the University of Utah Hospitals and Clinics, Dr. Kochenour says his institution has tried to emulate the anesthesiologists by concentrating more on identifying systemic errors and less on individual blame. But these efforts run headlong into thinking drummed into physicians since medical school, he says. "I don't think physicians are very good systems thinkers, by and large," he says. Many, especially surgeons, prize their independence, he says, and that makes it hard to achieve the kind of cooperation necessary to reduce errors.Best of luck. |
Tuesday, June 21, 2005
Grand Rounds XXXIX or 1:39......
Welcome to Grand Rounds, the weekly collection of the best of the medical blogosphere. Over the past few weeks medical bloggers have been getting a lot of exposure in the lay press. With the recentLA Times article and the guest editorial in USA Today penned by DB:
Another medical blogger is hitting the big time, being linked by The Corner and Captain's Quarters, to name a few. Their attention is focused on Orac's exceptional take-down of a Salon.com article on the thimerosal bogey-man and its' follow-up:
Do you recall a commercial for an insurance company that has a homeowner and plumber standing in a flooded basement. The plumber wants to get right to work but the homeowner wants his price, and the prices of his competitors? Well Insureblog informs us of a law in Illinois that would result in the publication of the cost of procedures to allow for consumer choice.
The Grunt Doc is happy in his work.
Speaking of surgeons my colleague out west has a discussion about the lack of open operative experience among today's resdients:
Dr. Rangel discusses the failure of TennCare with a horrific glimpse of the future:
Dr. Tony, however, visualizes a brighter future.
Nanotechnology at work.
Dr. Charles breaks down and engages in catblogging:
Maria comments on the male half of Hollywood's latest "Hot Couple" and his views on psychiatry:
The Health Business Blog explores the expansion of angioplasty in Massachusetts.:
In a series that potentially has an infinite life, Kevin MD provides us with several examples of how he "practiced defensive medicine today":
Speaking of a trip to the ED. The Cheerful Oncologist tells of a reaction to some of his potions:
JenSN tells the tale of a sickle cell patient after hip surgery and the difficulties of postop care.
Self exams for men go to the next level, courtesy of Mr. Sun.
He He.
From Clinical Cases, a post for the up-and-coming intern: How to put in a central line. Just don't forget the post-procedure film.
Has The Lancet become the Weekly World News of the peer-reviewed medical literature? Dr. Sanity tells us some from the Royal Society have taken the editors to the woodshed:
From last week's host: Red State Moron examines when physicians practice outside the "mainstream":
As an added bonus, the physician at the center of all this posts in the comments. An example of how those that stick up tend to be hammered down. In another post RSM opines on the recently introduced "Prenatally Diagnosed Conditions Awareness Act":
A new medblogger, Information is Free does a neurologic evaluation of cell-phone use while driving:
Ad Libitum takes a look at the misuse of the evidence-based moniker:
Dr. Emer hears a giant sucking sound. The sound of nurses leaving the Philippines:
Alois does an economic comparason between a medical degree and baseball cards.
The Medgadget guys ask us: one snake or two?
Enoch finds his choice of urgent care allows him to be the father he wants to be:
The Canadian National Health System suffered a blow from its' Supreme Court last week in a ruling that could expand the role of private health plans. Interested-Participant points out with pregnant women being sent to the states for care, maybe change is overdue:
The newly minted Dr. McBride offers up a discussion of the cost of prolonging life and wonders if longevity isn't everything:
Lastly, Dr. Rangel examines the re-emergence of the Terri Schiavo case and the political turmoil associated with it. Get your end-of-life wishes in writing. And make sure your whole family knows them!
This is the time of the year for transitions in medicine. Some such as
Doc Shazam and Dr. Lassiter are finishing their residencies and are moving on to "real jobs". Others are changing specialties. And a few more are beginning what may be the most challenging year of their lives. Best of luck to you all.
That's all folks. I had a tremendous amount of submissions this week, so if you didn't get included, my apologies. Next week Grand Rounds XXXX will be hosted by Mr. Williams at the Health Business Blog. Want to host? Drop a line to Dr. Genes. The archives may be found here.
Happy reading!! |
Welcome to Grand Rounds, the weekly collection of the best of the medical blogosphere. Over the past few weeks medical bloggers have been getting a lot of exposure in the lay press. With the recentLA Times article and the guest editorial in USA Today penned by DB:
Drug advertising results in more costly prescriptions. Few inexpensive drugs are advertised on TV. The commercials don't educate patients. Rather, they create a demand for a product based on an effective commercial rather than the patient's medical need.
Another medical blogger is hitting the big time, being linked by The Corner and Captain's Quarters, to name a few. Their attention is focused on Orac's exceptional take-down of a Salon.com article on the thimerosal bogey-man and its' follow-up:
The bottom line is that this article is indeed a humongous runny, stinking turd. Salon.com and Rolling Stone have let their readers down, contributed to the hysteria over a probably nonexistent link between mercury and autism, and utterly trashed their own credibility in the process. They've handed the antivaccination activists a significant propaganda victory and an article that they will be citing for years to come, frightening parents who wonder if vaccines are safe and wrongly adding to the guilt that parents of autistic children already feel by making them wonder if they were responsible for their child's condition
Do you recall a commercial for an insurance company that has a homeowner and plumber standing in a flooded basement. The plumber wants to get right to work but the homeowner wants his price, and the prices of his competitors? Well Insureblog informs us of a law in Illinois that would result in the publication of the cost of procedures to allow for consumer choice.
Interestingly, I noticed that the bill doesn't require the publication of success rates. In other words, one could find out the cheapest place for a given procedure, but not necessarily the best place. Remember, though, you get what you pay for.Indeed.
The Grunt Doc is happy in his work.
In the first two hours of my shift I've done more acute-care medicine than in a literal month of shifts, and it feels good. Occasionally I wonder about my career path, and today is one of the days I'm glad I'm an Emergency Physician.Give in to your anger! Join us! Become a trauma surgeon!
Speaking of surgeons my colleague out west has a discussion about the lack of open operative experience among today's resdients:
In the best of all possible worlds, newly minted surgeons would take jobs with older, more established surgeons that provide expertise and help ("mentoring," to use the current buzz word) -- here, again, I was and continue to be extremely fortunate in this regard. That is probably not attainable for many graduating residents. It is hard to conceive a situation where the RRC would mandate a certain percentage of cases to be done "open," either: can you imagine the consent form for patients at teaching facilities then ---- "if we determine that the resident helping with this operation has insufficient experience with the open technique, you'll get a bigger incision." That would be about as popular as Howard Dean at a NASCAR event.Again the law of unintended consequences strikes again.
Dr. Rangel discusses the failure of TennCare with a horrific glimpse of the future:
In 2009 President Hillary Clinton will resurrect her long dead dream of nationalized government health insurance. Medicare and Medicaid will be combined and expanded into a massive program that will cover every American. It will be administered by the states and further subdivided into "managed care regions" which will act similar to the old HMOs.And it's all downhill from there.
Dr. Tony, however, visualizes a brighter future.
The information from the analyzer was a blueprint for the exact "mechanical antibody" required to defeat Jane's virus. The recipe created the exact molecular milleu required for the assemblers in the capsule to replicate the mechanical antibody and continue to do so in Jane's GI system. These antibodies were bound to dendrimers, tree-like nanomolecules. On another branch were nutrients required by the specific virus that was infecting Jane. As the virus concentrated the nutrients, they unknowingly incorporated instructions into their own RNA that changed them from pathologic to healthful.
Nanotechnology at work.
Dr. Charles breaks down and engages in catblogging:
"That little scamp!" the old woman exclaimed to me, gently rubbing the wound on her hand that I had just finished cleaning. "I'll take all these antibiotics if you say I should, but that vicious little kitty is going to get it!"
Maria comments on the male half of Hollywood's latest "Hot Couple" and his views on psychiatry:
If Tom Cruise has not ever personally suffered from mental illness, it is my sincere hope that he is grateful for that blessing. His faith in Scientology is steadfast, but his proselytization of the merits of his faith, particularly in the realm of (anti) psychiatry, only reveals his ignorance and lack of empathy for those who do not share in his good fortune and blessings.
The Health Business Blog explores the expansion of angioplasty in Massachusetts.:
But why not take things a step further? Include the existing academic centers and relevant community hospitals in the study. At the end of five years, certify or re-certify only the top half of hospitals to perform the procedure, regardless of whether they are academic or community based. That kind of competition could spur real improvements for Massachusetts patients.
In a series that potentially has an infinite life, Kevin MD provides us with several examples of how he "practiced defensive medicine today":
I may have lost a patient, and drove up costs by advising a probable conjunctivitis to go to the ER, but at least there is zero possibility of being sued over this. It's a trade I'll make every time.Me too, brother.
Speaking of a trip to the ED. The Cheerful Oncologist tells of a reaction to some of his potions:
It didn't take a session with an IBM mainframe to place the puzzle pieces together and come up with a plan. Let's remember folks - we doctors are skilled in the art of leaving no stone unturned when it comes to finding a diagnosis. Why is that, one might ask? Well, given the menacing cloud of litigation that doctors practice under these days, one would understand with Zeus-like clarity why I rushed this patient to the emergency room. The decision was justified if one notices the overlap between my patient's symptoms and those of a major perturbation of the old ticker. Hypersensitivity reactions that are minor can be managed at the bedside by turning off the infusion and treating with Benadryl, corticosteroids, oxygen, IV fluids. Major hypersensitivity reactions (called anaphylaxis) are treated like a cardiac arrest - no head-scratching over that diagnosis, eh? My patient's symptoms were atypical for an allergic reaction, and rather than assume that the most likely diagnosis was the actual diagnosis, I checked for other serious problems that could have lethal consequences if undiscovered.
JenSN tells the tale of a sickle cell patient after hip surgery and the difficulties of postop care.
Self exams for men go to the next level, courtesy of Mr. Sun.
I feel it is very important for men to be examined regularly, so I'd like to take this opportunity to walk everyone through the process I just completed in the hopes it will lower the barriers of fear surrounding this very necessary medical procedure.
He He.
From Clinical Cases, a post for the up-and-coming intern: How to put in a central line. Just don't forget the post-procedure film.
Has The Lancet become the Weekly World News of the peer-reviewed medical literature? Dr. Sanity tells us some from the Royal Society have taken the editors to the woodshed:
It is truly medical scaremongering to report the results of badly designed studies; or to report the results in a manner designed to frighten people. The only possible purpose of such studies is the self-aggrandizement of the authors and publishers--who hold their press conferences and intone seriously about the "risks" posed by this or that. In the case of vaccines, more people will die and suffer because they didn't get the vaccine, than the opposite.
From last week's host: Red State Moron examines when physicians practice outside the "mainstream":
Fellow Wilmington obstetrician Dr. Joshua Vogel said though she was considered too set in her ways or a renegade by some doctors, he admired her talents to deliver naturally in situations when other doctors would have automatically pushed for a c-section. "She was a valuable asset for patients," he said.And draws the scrutiny of "the committee":
The first letter, written by Dr. Cobern Peterson, chairman of the Professional Review Committee, stated "concerns" regarding her practice. They include higher than average infant birth weights, much lower than average c-section rates and later than average gestational age of neonates at delivery.
The letter states "the main concern reiterated several times was an overall practice attitude rather than any individual case."
As an added bonus, the physician at the center of all this posts in the comments. An example of how those that stick up tend to be hammered down. In another post RSM opines on the recently introduced "Prenatally Diagnosed Conditions Awareness Act":
I don't disagree. It is challenge. It's a challenge to tell a woman that her baby has Trisomy 18. Or Trisomy 13. Or a hypoplastic left heart. And the authors message is constructive. But does it require federal legislation? On the basis of 141 respondents to a survey, we need federal legislation because, in essence, we are not doing our jobs? Am I understanding this correctly?But it's for the children!!!!
A new medblogger, Information is Free does a neurologic evaluation of cell-phone use while driving:
One of the bedside tests we do of memory is to give someone a series of digits, after which the person is supposed to repeat the sequence. Most people can repeat a maximum of 7-9 digits without making a mistake. What this should give you is a sense of how much information anyone can handle moment-to-moment; it's not muchHow about those Bluetooth headsets that make you look like Mr. Spock?
Ad Libitum takes a look at the misuse of the evidence-based moniker:
It's as if just including the phrase "evidence-based" adds a patina of respectability (and superiority) to the title of a paper or a policy. There's also no denying that sometimes including this phrase conveys an attitude of being holier-than-thou. It's like saying "Hey, I'm evidence-based, so you can't say anything against me." Never mind that in many cases this phrase is used very loosely and quite differently from the original intent behind it.
Dr. Emer hears a giant sucking sound. The sound of nurses leaving the Philippines:
In the last 10 years, the Philippines exported close to 90,000 nurses overseas.The top scorer on the physician's exam has announced he too, will enter nursing.
In the last four years, 3,500 doctors left the country to take on nursing posts abroad.
The number 1 course choice here is now Nursing. I have friend lawyers, engineers, and yes, doctors who are all shifting to nursing to work abroad.
Alois does an economic comparason between a medical degree and baseball cards.
The Medgadget guys ask us: one snake or two?
So what does the staff of Asclepius symbolize? Dr. Blayley speculates the image's origin might arise from the practice of removing subcutaneous parasites. The worms would be pulled from an incision and wound around a stick -- the practice was so common that doctors may have come to advertise their services by depicting this procedure.Imagine that in a DTC ad!!
Enoch finds his choice of urgent care allows him to be the father he wants to be:
After a lot of deferred gratification (4 y med school, 3 y residency, 2 y internet startup, 2 years pre-partner busyness) i'm now able to split my 40 hours/week into 3 shifts, 2 X 18 hour ones and one shorter 5-10 hour one. The rest of my time i spend at home with the kids, swimming, or going out to our preschool co-op, or parks, or playgroups.Sign me up!!!
The Canadian National Health System suffered a blow from its' Supreme Court last week in a ruling that could expand the role of private health plans. Interested-Participant points out with pregnant women being sent to the states for care, maybe change is overdue:
The phrase "no room for her last week in hospitals in Toronto, London, Hamilton and Kingston" is disturbing and probably an indication that the current system is already functioning at maximum capacity, i.e. no room for another baby. It's not exactly clear why there isn't public outrage. Sending patients to another facility is common and understandable. Sending patients to another country because there's "no room at the inn" means that the entire health care system is deficient
The newly minted Dr. McBride offers up a discussion of the cost of prolonging life and wonders if longevity isn't everything:
I'd like to pose a question for the two, in hopes that they keep this debate going. Don't you have to recognize the non-mortality benefits of medical care? Medicine doesn't always make us live longer, but it can make us live better. Preventing a lot of non-fatal heart attack may not change average mortality that much, but it sure makes life quality better. And then there is psychiatry, which can provide a lot of benefits at virtually no decreases in mortality. And what about plastic surgery, arthritis, orthopedics and physical therapy, dentistry; the list goes on. Same thing. When you actually sit down and separate all the fields of medicine and health care, very few sectors are actually even aiming for improved quantity of life. A good portion of surgery and pediatrics and a smaller part of internal medicine (mostly cardiology and nephrology) have shown good headway by this measure. But to ignore the marginal benefits of quality of life brought by some health care sectors underestimates the overall marginal benefits. In other words, life expectancy gains aren't everything.
Lastly, Dr. Rangel examines the re-emergence of the Terri Schiavo case and the political turmoil associated with it. Get your end-of-life wishes in writing. And make sure your whole family knows them!
This is the time of the year for transitions in medicine. Some such as
Doc Shazam and Dr. Lassiter are finishing their residencies and are moving on to "real jobs". Others are changing specialties. And a few more are beginning what may be the most challenging year of their lives. Best of luck to you all.
That's all folks. I had a tremendous amount of submissions this week, so if you didn't get included, my apologies. Next week Grand Rounds XXXX will be hosted by Mr. Williams at the Health Business Blog. Want to host? Drop a line to Dr. Genes. The archives may be found here.
Happy reading!! |
Monday, June 20, 2005
Help the Doctor!!!!!
Don't forget to send in your submissions for tomorrow's Grand Rounds by 9 PM EDT tonight!! |
Don't forget to send in your submissions for tomorrow's Grand Rounds by 9 PM EDT tonight!! |
Saturday, June 18, 2005
Call for Submissions....
Next weeks Grand Rounds will be held here. Please submit your posts, or those by others that catch your eye by 9:00 PM EDT June 20th, 2005. Leave links in the comments or email them to me: cut_to_cure-at-hotmail dot com.
Want to host in the future? Contact the newly minted Dr. Genes. |
Next weeks Grand Rounds will be held here. Please submit your posts, or those by others that catch your eye by 9:00 PM EDT June 20th, 2005. Leave links in the comments or email them to me: cut_to_cure-at-hotmail dot com.
Want to host in the future? Contact the newly minted Dr. Genes. |
Scan'em All and let God Sort Them Out II.....
A trio of articles again from this month's Journal of Trauma. The first:Spiral Computed Tomography for the Diagnosis of Cervical, Thoracic, and Lumbar Spine Fractures: Its Time has Come.
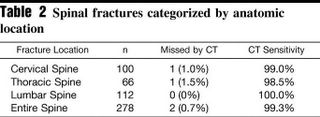
The sensitivity for plan radiographs from the study population are: 67% (6/9) for cervical fractures, 64% (7/11) for thoracic fractures, and 69% (11/16) for lumbar fractures. The next:Helical Computed Tomographic Scanning for the Evaluation of the Cervical Spine in the Unconscious, Intubated Trauma Patient.
The results of plain radiography:

Compared to helical CT:

And lastly, a meta-analysis:Computed Tomography Versus Plain Radiography to Screen for Cervical Spine Injury: A Meta-Analysis.
There have been other studies analyzing the accuracy of using the imaged vertebrae during chest and abdominal CT as a screening tool. Others have described the use of the initial "scout" views for that purpose as well. As the technology has advanced the concept of the "pan-scan": a CT of the head, total spine, chest, abdomen and pelvis has gained wider acceptance. Products such as the Statscan promise to bring such technology from the CT room to the resuscitation bay, as it has at the University of Maryland Shock-Trauma Center.
My own practice is to obtain CT scans of the cervical spine if the initial series is inadequate or is suspicious. I have not yet utilized spinal CT as a routine tool to evaluate the symptomatic or unconscious/intoxicated patient, but given these studies, I may begin to do so. |
A trio of articles again from this month's Journal of Trauma. The first:Spiral Computed Tomography for the Diagnosis of Cervical, Thoracic, and Lumbar Spine Fractures: Its Time has Come.
Background: Although the traditional method of diagnosing spine fractures (SF) has been plain radiography, Spiral Computed Tomography (SCT) is being used with increasing frequency. Our institution adopted SCT as the primary modality for the diagnosis of SF. The purpose of this study was to determine whether SCT scan can be used as a stand-alone diagnostic modality in the evaluation of SF.
Methods: Retrospective review of all blunt trauma patients over a two year period (1/01 - 12/02). Patients with neck pain, back pain, or spine tenderness underwent SCT of the symptomatic region. Patients who were unconscious or intoxicated underwent screening SCT of the entire spine. SCT was performed using 5 mm axial cuts with three-dimensional reconstructions in sagittal and coronal planes. Patients with a discharge diagnosis of cervical, thoracic, or lumbar SF were identified from the trauma registry by ICD-9 codes.
Results: There were 3,537 blunt trauma patients evaluated, with 236 (7%) sustaining a cervical, thoracic, or lumbar SF. Forty-five patients (19%) sustained a SF in more than one anatomic region. SCT missed SF in two patients. The cervical SF missed by SCT was a compression fracture identified by magnetic resonance imaging and was treated with a rigid collar. The thoracic SF missed by SCT was also a compression fracture identified on plain radiographs and required no treatment.
Conclusions: SCT of the spine identified 99.3% of all fractures of the cervical, thoracic, and lumbar spine, and those missed by SCT required minimal or no treatment. SCT is a sensitive diagnostic test for the identification of SF. Routine plain radiographs of the spine are not necessary in the evaluation of blunt trauma patients.
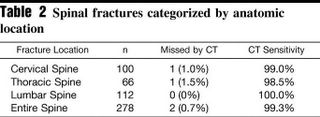
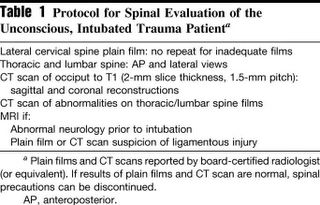
The sensitivity for plan radiographs from the study population are: 67% (6/9) for cervical fractures, 64% (7/11) for thoracic fractures, and 69% (11/16) for lumbar fractures. The next:Helical Computed Tomographic Scanning for the Evaluation of the Cervical Spine in the Unconscious, Intubated Trauma Patient.
Background: Assessment of the spine in the unconscious trauma patient is limited by an inadequate clinical examination. The potential of a missed unstable disc or ligamentous injury results in many patients remaining immobilized in critical care units for prolonged periods.The protocol does not appear as strict as the first study:
Methods: This study evaluates helical computed tomographic (CT) scanning of the whole cervical spine as part of a spinal assessment and clearance protocol.
Results: Four hundred thirty-seven unconscious, intubated, blunt trauma patients underwent CT scanning of the cervical spine. Sixty-one patients had a cervical spine injury and 31 (7.0%) were unstable. CT scanning had a sensitivity of 98.1%, a specificity of 98.8%, and a negative predictive value of 99.7%. There were no missed unstable injuries. In contrast, an adequate lateral cervical spine film detected only 24 injuries (14 unstable), with a sensitivity of 53.3%.
Conclusion: Helical CT scanning of the cervical spine allows rapid and safe evaluation of the cervical spine in the unconscious, intubated trauma patient.
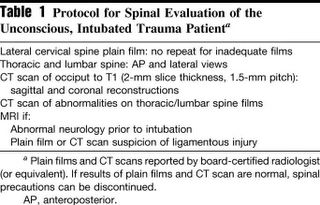
The results of plain radiography:

Compared to helical CT:

And lastly, a meta-analysis:Computed Tomography Versus Plain Radiography to Screen for Cervical Spine Injury: A Meta-Analysis.
Background: To compare the test performance of plain radiography and computed tomography (CT) in the detection of patients with cervical spine injuries following blunt traumatic events among those patients determined to require screening radiography.
Methods: We conducted a MEDLINE search for articles published from January 1995 through June 2004, manually reviewed bibliographies, and hand searched four journals. Studies were included if they contained data on the performance of both plain radiography and CT in the detection of patients with blunt cervical spine injuries. Both authors screened titles and abstracts identified by the search and seven of the 712 articles met all inclusion criteria. Both authors independently abstracted data from these seven studies and disagreements were resolved by mutual agreement.
Results: Patient entry criteria were highly variable for each study and there were no randomized controlled trials. For identifying patients with cervical spine injury, the pooled sensitivity for cervical spine plain radiography was 52% (95% CI 47, 56%) and for CT was 98% (95% CI 96, 99%). The test for heterogeneity suggests that significant differences exist between studies in the measurement of the sensitivity for plain radiography (p = 0.07). Due to limitations of the gold standard tests in each study, a calculation of a combined specificity was not possible.
Conclusion: Despite the absence of a randomized controlled trial, ample evidence exists that CT significantly outperforms plain radiography as a screening test for patients at very high risk of cervical spine injury and thus CT should be the initial screening test in those patients with a significantly depressed mental status. There is insufficient evidence to suggest that cervical spine CT should replace plain radiography as the initial screening test for less injured patients who are at low risk for cervical spine injury but still require a screening radiographic examination.
There have been other studies analyzing the accuracy of using the imaged vertebrae during chest and abdominal CT as a screening tool. Others have described the use of the initial "scout" views for that purpose as well. As the technology has advanced the concept of the "pan-scan": a CT of the head, total spine, chest, abdomen and pelvis has gained wider acceptance. Products such as the Statscan promise to bring such technology from the CT room to the resuscitation bay, as it has at the University of Maryland Shock-Trauma Center.
My own practice is to obtain CT scans of the cervical spine if the initial series is inadequate or is suspicious. I have not yet utilized spinal CT as a routine tool to evaluate the symptomatic or unconscious/intoxicated patient, but given these studies, I may begin to do so. |
Thursday, June 16, 2005
Share the Wealth...
Or pass the buck. From The Journal of Trauma:Workload Redistribution: A New Approach to the 80-Hour Workweek.

And hours:

There were no statisically significant difference in the number of missed injuries between the pre and post sample periods.
This paper was presented at the AAST meeting and inspired a lively discussion about the role of the trauma service and the specialist surgeon:
In reply(emphasis mine)....
So will we have a "captain-less" ship? |
Or pass the buck. From The Journal of Trauma:Workload Redistribution: A New Approach to the 80-Hour Workweek.
Background: The new Accreditation Council for Graduate Medical Education-mandated 80-hour resident work week has resulted in busy trauma services struggling to meet these strict guidelines, or face loss of accreditation.They analyzed the volume of trauma admissions between July and December 2002 (pre) and July to December 2003 (post). After July 2003 isolated neuro and orthopedic injuries would be admitted to the respective service. The six month totals were 543 and 549 patients. (my level II trauma center cares for almost as many patients). It seems they did reduce volume and improve workhour compliance, but altering the dynamic of the trauma service:
Methods: Beginning in July 2003, our Level I trauma service began a policy of direct admission of isolated neurosurgical or orthopedic injuries to the specific subspecialty service after complete evaluation by the trauma service in the emergency department for associated injuries. Complications, missed injuries, delayed diagnoses, and admission rates were compared in two 6-month periods: PRE, before the policy change; and POST, after the new policy had been instituted. Resident work hours were likewise compared over the two time periods.
Results: Selected single-system injury admission to subspecialty services resulted in a 15% reduction in admissions to the trauma service. There were no significant differences in the overall complication rate, delayed diagnoses, or missed diagnoses between the PRE and POST time periods. Overall, there was a 9.7% reduction in resident work hours (p = 0.45; analysis of variance) between the PRE and POST periods, which allowed them, on average, to meet the Accreditation Council for Graduate Medical Education 80-hour workweek mandate.
Conclusion: Direct admission of patients with isolated injuries to subspecialty services is safe and decreases the workload of residents on busy trauma services.
It has been tradition that the trauma surgeon is captain of the ship, responsible for the oversight and care of the trauma patient. As a consequence of this tradition, all trauma patients are admitted for observation to the trauma services for at least 24 to 48 hours. During this period, subspecialty involvement is limited to a consultative role. The purpose of the period of observation is to avoid missed injuries and to expedite workup and diagnosis.The patients are initially evaluated by the trauma team and "farmed out" if the criteria are met. The results for admissions:
In 2003, the Accreditation Council for Graduate Medical Education (ACGME) mandated that residents in surgical specialties work no more than 80 hours per week. This ACGME mandate was enforced in July 2004. Because the trauma service is often the busiest surgical service in a hospital, innovative approaches to meet the 80-hour workweek mandate have been tried, including night float services, limited teaching services, and the involvement of midlevel providers in the care of the trauma patient.
The trauma service at Fletcher Allen Health Care/University of Vermont has been an American College of Surgeons-verified Level I trauma service since 1993. To meet the ACGME 80-hour workweek mandate, we altered our trauma protocol. We allowed selected patients with single-system injuries to be admitted to subspecialty services without a period of observation on the trauma service. This direct admission to subspecialty services was predicated on a full trauma evaluation by the trauma team in the emergency department at the time of admission. Our system incorporated a definition of single-system injury in which the main injury requiring subspecialty service admission had an Abbreviated Injury Scale (AIS)1 score of 3 or greater, with no other injuries of AIS score than 2. We hypothesized that this policy would reduce trauma resident workload and, in addition, would not increase delayed diagnoses or missed diagnoses.

And hours:

There were no statisically significant difference in the number of missed injuries between the pre and post sample periods.
This paper was presented at the AAST meeting and inspired a lively discussion about the role of the trauma service and the specialist surgeon:
Dr. Fred A. Luchette .....You have called this change in admitting service workload redistribution. Is it really a redistribution or just a shift of the workload to residents on the orthopedic and neurosurgery services? How has this impacted on their ability to comply with the 80-hour workweek? What effect has this practice had on the relationship between the residents on the various services? Do the orthopedic and neurosurgery residents feel the trauma service is dumping on them? What other changes were made by the general surgery residency program director so the residents would be compliant with the work hour restrictions? Convince me that the residents would not have been compliant with the 80-hour policy without this change by the trauma serviceConcerns over complication and the "presence" of the trauma service:
Dr. Sheldon Brotman.... You know one of the requirements in the gold book is that there should be a visible trauma service. The problem I have is when these patients go into orthopedics or neurosurgery, frequently the trauma residents become absolutely invisible. Although patients may go to subspecialty services the next day or two, I think trauma teams need to make rounds. They need to go back over the patient and look for missed injuries. In my own experience, it's frequently difficult to enforce that.......
Somehow, the complications that occur in orthopedics and neurosurgery aren't collected quite as carefully. Also, I don't think that the discharge process is really quite as facile in the other services either.
In reply(emphasis mine)....
Are we shifting the work to orthopedics and neurosurgery? Yes, but let's look at this. At our institution, over 90% of the operations performed on trauma patients are performed by subspecialty services.
If they are going to be performing the operations, isn't it appropriate that they take care of the patients afterward? The subspecialties can't have it both ways.
If they want to perform the operations, then they should take care of the patients in the perioperative period. Alternatively, if they are going to remain on our service, then maybe we should be performing some of these procedures, such as Dr. Cryer suggested in his presidential address.
I don't need to remind anyone in this room what a powerful negative disincentive it is for a medical student or resident, contemplating a career in trauma surgery, to see the trauma surgeons taking care of orthopedic or neurosurgical patients on their service after the subspecialty services have performed a huge operation with a huge professional component attached to it. To me, this borders almost on itinerant surgery.
So will we have a "captain-less" ship? |
Tuesday, June 14, 2005
Grand Rounds 1:38......
The Red State Moron gives us Grand Rounds XXXVIII, as well as an easier way to number them, as the Roman numerals are becoming cumbersome.
In addition I will be hosting Grand Rounds 1:39 (or XXXIX)next week. Please submit posts to: cut_to_cure-at-hotmail dot com. by 9PM EDT on June 20th, 2005. |
The Red State Moron gives us Grand Rounds XXXVIII, as well as an easier way to number them, as the Roman numerals are becoming cumbersome.
In addition I will be hosting Grand Rounds 1:39 (or XXXIX)next week. Please submit posts to: cut_to_cure-at-hotmail dot com. by 9PM EDT on June 20th, 2005. |
Monday, June 13, 2005
The Company Man...
Via hcrenewal and The Retired Doc comes this story from The Miami Herald:AMA pursues doctor hiring reform:
Of course, when the AMA goes off and does something, somebody's going to get mad:
So hospitals and companies employ physicians because:
Some physicians (especially younger ones) find negotiating the particulars of insurance contracts, office management, and other business aspects of medicine difficult. By taking employment with hospitals or companies they have strength in numbers and someone else to handle management. Such options will become more appealing as the anticipated/dreaded "shift-work" mentality associated with the 80-hour workweek becomes entrenched.
The dynamics of hospitals have changed. The advent of specialty hospitals and ambulatory surgery centers have made serving on the medical staff of a community general hospital optional. Many surgical specialists have stopped doing so. In order to provide the service in a reliable fashion hospitals have had to employ these physicians.
Under provisions of the Stark Law, hospitals cannot provide assistance with liability insurance. So many, such as the neurosurgeons above, find refuge in hospital employment. Some enjoy limited liability as government employees under those circumstances.
The uninsured and Medicaid patients need to have someplace to go, as many in private practice will not see those patients. Hospital clinics, staffed by hospital employed physicians, can provide that service.
What of physicians who work for locum tenens firms?
What strikes me is that the AMA is proposing a policy that would restrict physician career options. Of course, the AMA does engage in silliness from time to time. |
Via hcrenewal and The Retired Doc comes this story from The Miami Herald:AMA pursues doctor hiring reform:
In a move that could have widespread effects on the nation's healthcare industry, the American Medical Association's Board of Trustees is recommending the development of proposed legislation that would forbid corporations and hospitals from directly employing physicians.
Joseph Heyman, a Massachusetts gynecologist who is an AMA trustee, said the board acted because ``we don't want to have corporations or anybody using their concerns about finance to influence the relationship between a patient and a physician. We want the physicians to . . . make the best choices for the patients.''
Of course, when the AMA goes off and does something, somebody's going to get mad:
''This doesn't make sense,'' said Frank Sacco, chief executive of the South Broward Hospital District, which employs more than 100 doctors. ``They're completely out of touch with the physicians of this country.''Some of the reasons that hospitals or companies employ physicians:
''They're trying to put a genie back in the bottle that has been out for a long time,'' said Stephen J. Desnick, chief executive of Sterling Healthcare, which employs 1,000 doctors, mostly in emergency rooms. He called the AMA ``extraordinarily conservative. They're just not in line with what's happening.''
Corporations employing physicians have been growing in recent years as doctors in solo or small-group practices have found it difficult to make a go of it because of rising costs and squeezed reimbursements from managed care plans. Pediatrix specializes in the treatment of newborns in hospitals. Sterling focuses on emergency room doctors.
Both North Broward and South Broward Hospital districts now employ neurosurgeons because they find its the only way to get their services in their operating rooms. The neurosurgeons, who can't afford or can't get malpractice premiums, thus become government employees and have limited liability in lawsuits.
Sacco, head of the South District, says he finds it necessary to hire a broad range of specialists, including 15 or 20 primary-care doctors to handle the uninsured in public clinics.
So hospitals and companies employ physicians because:
Some physicians (especially younger ones) find negotiating the particulars of insurance contracts, office management, and other business aspects of medicine difficult. By taking employment with hospitals or companies they have strength in numbers and someone else to handle management. Such options will become more appealing as the anticipated/dreaded "shift-work" mentality associated with the 80-hour workweek becomes entrenched.
The dynamics of hospitals have changed. The advent of specialty hospitals and ambulatory surgery centers have made serving on the medical staff of a community general hospital optional. Many surgical specialists have stopped doing so. In order to provide the service in a reliable fashion hospitals have had to employ these physicians.
Under provisions of the Stark Law, hospitals cannot provide assistance with liability insurance. So many, such as the neurosurgeons above, find refuge in hospital employment. Some enjoy limited liability as government employees under those circumstances.
The uninsured and Medicaid patients need to have someplace to go, as many in private practice will not see those patients. Hospital clinics, staffed by hospital employed physicians, can provide that service.
What of physicians who work for locum tenens firms?
What strikes me is that the AMA is proposing a policy that would restrict physician career options. Of course, the AMA does engage in silliness from time to time. |
Sunday, June 12, 2005
Friday, June 10, 2005
Blast from the Past......
From Adult ADD Strengths comes a link to this Livejournal site with vintage drug adds. "Mother's Little Helpers" seemed to be quite popular.
I found one that caught my fancy. Here is the "Operating Room of Tomorrow":
 |
|
From Adult ADD Strengths comes a link to this Livejournal site with vintage drug adds. "Mother's Little Helpers" seemed to be quite popular.
I found one that caught my fancy. Here is the "Operating Room of Tomorrow":
Thursday, June 09, 2005
Tales from the Trauma Service XII......
20-ish year old stabbed in the left lower chest and upper abdomen. He is intoxicated and hemodynamicaly stable. This injury is one that is best able to be approached with a laparoscope. Off to the operating room:

The view from afar....

Up close. This photo from the laparoscopic camera. The superior laceration was where trouble would arise.

Hey what's this??

Why, it's Dr. Parker's finger!!! This can be repaired laparoscopicaly but given the early-morning hour and personnel present I judged that the best approach would be the conventional open one.
Call me a chicken....
20-ish year old stabbed in the left lower chest and upper abdomen. He is intoxicated and hemodynamicaly stable. This injury is one that is best able to be approached with a laparoscope. Off to the operating room:

The view from afar....

Up close. This photo from the laparoscopic camera. The superior laceration was where trouble would arise.

Hey what's this??

Why, it's Dr. Parker's finger!!! This can be repaired laparoscopicaly but given the early-morning hour and personnel present I judged that the best approach would be the conventional open one.
Call me a chicken....
Labels: Tales from the Trauma Service
|Wednesday, June 08, 2005
An Innocent Abroad......
From Opinion Journal: Fox News host David Asman describes his wife's experience in the British and American health system:There's No Place Like Home Mr. Asman has nothing but good things to say about the people who took care of his wife:
Defensive medicine seems to be absent from Great Britain:
So how much did it cost?
O.K., who wants to sign up first? |
From Opinion Journal: Fox News host David Asman describes his wife's experience in the British and American health system:There's No Place Like Home Mr. Asman has nothing but good things to say about the people who took care of his wife:
The emergency workers who came within five minutes were wonderful. The two young East Enders looked and sounded for all the world like a couple of skinhead soccer fans, cockney accents and all. But their professionalism in immediately stabilizing my wife and taking her vitals was matched with exceptional kindness. I was moved to tears to see how comforting they were both to my wife and to me. As I was to discover time and again in the British health system, despite the often deplorable conditions of a bankrupt infrastructure, British caregivers--whether nurses, doctors, or ambulance drivers--are extraordinarily kind and hardworking. Since there's no real money to be made in the system, those who get into public medicine do so as a pure vocation.And the collaborative nature of care was impressive:
As for the caliber of medicine practiced at Queen's Square, we were quite impressed at the collegiality of the doctors and the tendency to make medical judgments based on group consultations. There is much better teamwork among doctors, nurses and physical therapists in Britain. In fact, once a week at Queen's Square, all the hospital's health workers--from high to low--would assemble for an open forum on each patient in the ward. That way each level knows what the other level is up to, something glaringly absent from U.S. hospital managementBut the facilities left much to be desired:
When I covered Latin America for The Wall Street Journal, I'd visit hospitals, prisons and schools as barometers of public services in the country. Based on my Latin American scale, Queen's Square would rate somewhere in the middle. It certainly wasn't as bad as public hospitals in El Salvador, where patients often share beds. But it wasn't as nice as some of the hospitals I've seen in Buenos Aires or southern Brazil. And compared with virtually any hospital ward in the U.S., Queen's Square would fall short by a mile.There is also the technology gap:
The equipment wasn't ancient, but it was often quite old. On occasion my wife and I would giggle at heart and blood-pressure monitors that were literally taped together and would come apart as they were being moved into place. The nurses and hospital technicians had become expert at jerry-rigging temporary fixes for a lot of the damaged equipment. I pitched in as best as I could with simple things, like fixing the wiring for the one TV in the ward. And I'd make frequent trips to the local pharmacies to buy extra tissues and cleaning wipes, which were always in short supply.
For example, when we returned to the U.S. we discovered that treatment exists for thwarting the effects of blood clots in the brain if administered shortly after a stroke. Such treatment was never mentioned, even after we were admitted to the neurology hospital. Indeed, the only medication my wife was given for a severe stroke was a daily dose of aspirin. Now, treating stroke victims is tricky business. My wife had a low hemoglobin count, so with all the medications in the world, she still might have been better off with just aspirin. But consultations with doctors never brought up the possibilities of alternative drug therapies.
Defensive medicine seems to be absent from Great Britain:
There is also much less of a tendency in British medicine to make decisions on the basis of whether one will be sued for that decision. This can lead to a much healthier period of recuperation. For example, as soon as my wife was ambulatory, I was determined to get her out of the hospital as much as possible. Since a stroke is all about the brain, I wanted to clear her head of as much sickness as I could. We'd take off in a wheelchair for two-hour lunches in the lovely little park outside, and three-hour dinners at a nice Japanese restaurant located at a hotel down the street. I swear those long, leisurely dinners, after which we'd sit in the lobby where I'd smoke a cigar and we'd talk for another hour or so, actually helped in my wife's recovery. It made both of us feel, well, normal. It also helped restore a bit of fun in our relationship, which too often slips away when you just see your loved one in a hospital setting.The Asmans also get to see how the other half live during a trip to a private hospital:
Now try leaving a hospital as an inpatient in the U.S. In fact, we did try and were frustrated at every step. You'd have better luck breaking out of prison. Forms, permission slips and guards at the gate all conspire to keep you in bounds. It was clear that what prevented us from getting out was the pressing fear on everyone's part of getting sued. Anything happens on the outside and folks naturally sue the hospital for not doing their job as the patient's nanny.
Why are the Brits so less concerned about being sued? I can only guess that Britain's practice of forcing losers in civil cases to pay for court costs has lessened the number of lawsuits, and thus the paranoia about lawsuits from which American medical services suffer.
Before she could travel back home, my wife needed to have the weak wall in her heart fortified with a metal clamp. The procedure is minimally invasive (a catheter is passed up to the heart from a small incision made in the groin), but it requires enormous skill. The cardiologist responsible for the procedure, Seamus Cullen, worked in both the public system and as a private clinician. He informed us that the waiting line to perform the procedure in a public hospital would take days if not weeks, but we could have the procedure done in a private hospital almost immediately. Since we'd already been separated from our 12-year-old daughter for almost a month, we opted to have the procedure done (with enormous assistance from my employer) at a private hospital.Ms. Asman then returns to the States for her rehab.
Checking into the private hospital was like going from a rickety Third World hovel into a five-star hotel. There was clean carpeting, more than enough help, a private room (and a private bath!) in which to recover from the procedure, even a choice of wines offered with a wide variety of entrees. As we were feasting on our fancy new digs, Dr. Cullen came by, took my wife's hand, and quietly told us in detail about the procedure. He actually paused to ask us whether we understood him completely and had any questions. Only one, we both thought to ask: Is this a dream?
So how much did it cost?
But what of the bottom line? When I received the bill for my wife's one-month stay at Queen's Square, I thought there was a mistake. The bill included all doctors' costs, two MRI scans, more than a dozen physical therapy sessions, numerous blood and pathology tests, and of course room and board in the hospital for a month. And perhaps most important, it included the loving care of the finest nurses we'd encountered anywhere. The total cost: $25,752. That ain't chump change. But to put this in context, the cost of just 10 physical therapy sessions at New York's Cornell University Hospital came to $27,000--greater than the entire bill from British Health Service!A way I have read about how to compare this is that even the exchange rate today is 1 pound= $1.82 the purchasing power between the pound and the dollar is roughly equal. That is a pair of shoes that cost $70 here will go for 70 pounds over there, but I digress. Back to the article:
There is something seriously out of whack about 10 therapy sessions that cost more than a month's worth of hospital bills in England. Still, while costs in U.S. hospitals might well have become exorbitant because of too few incentives to keep costs down, the British system has simply lost sight of costs and incentives altogether. (The exception would appear to be the few remaining private clinics in Britain. The heart procedure done in the private clinic in London cost about $20,000.)
"Free health care" is a mantra that one hears all the time from advocates of the British system. But British health care is not "free." I mentioned the cost of living in London, which is twice as high for almost any good or service as prices in Manhattan. Folks like to blame an overvalued pound (or undervalued dollar). But that only explains about 30% of the extra cost. A far larger part of those extra costs come in the hidden value-added taxes--which can add up to 40% when you combine costs to consumers and producers. And with salaries tending to be about 20% lower in England than they are here, the purchasing power of Brits must be close to what we would define as the poverty level. The enormous costs of socialized medicine explain at least some of this disparity in the standard of living.
As for the quality of British health care, advocates of socialized medicine point out that while the British system may not be as rich as U.S. heath care, no patient is turned away. To which I would respond that my wife's one roommate at Cornell University Hospital in New York was an uninsured homeless woman, who shared the same spectacular view of the East River and was receiving about the same quality of health care as my wife. Uninsured Americans are not left on the street to die.
O.K., who wants to sign up first? |
Does the 80-hour Workweek Improve Safety?????
From the Annals of Surgery: Resident Work Hour Limits and Patient Safety
Three sets of hospitals were studied, New York teaching hospitals, New York non-teaching hospitals ,and California teaching hospitals. This was done to provide both geographic proximity during the time in question as well as teaching hospitals not affected by workhour limits. This study does a better job of telling us "this is the way it is" than "why is it this way"?
That paper was discussed here. And this is a point I have made repeatedly concerning the 80-hour workweek:
More to come, I'm sure. |
From the Annals of Surgery: Resident Work Hour Limits and Patient Safety
Objective: This study evaluates the effect of resident physician work hour limits on surgical patient safety.
Background: Resident work hour limits have been enforced in New York State since 1998 and nationwide from 2003. A primary assumption of these limits is that these changes will improve patient safety. We examined effects of this policy in New York on standardized surgical Patient Safety Indicators (PSIs).
Methods: An interrupted time series analysis was performed using 1995 to 2001 Nationwide Inpatient Sample data. The intervention studied was resident work hour limit enforcement in New York teaching hospitals. PSIs included rates of accidental puncture or laceration (APL), postoperative pulmonary embolus or deep venous thrombosis (PEDVT), foreign body left during procedure (FB), iatrogenic pneumothorax (PTX), and postoperative wound dehiscence (WD). PSI trends were compared pre- versus postintervention in New York teaching hospitals and in 2 control groups: New York nonteaching hospitals and California teaching hospitals.
Results: A mean of 2.6 million New York discharges per year were analyzed with cumulative events of 33,756 (APL), 36,970 (PEDVT), 1,447 (FB), 10,727 (PTX), and 2,520 (WD). Increased rates over time (expressed per 1000 discharges each quarter) were observed in both APL (0.15, 95% confidence interval, 0.09-0.20, P<0.05)
Three sets of hospitals were studied, New York teaching hospitals, New York non-teaching hospitals ,and California teaching hospitals. This was done to provide both geographic proximity during the time in question as well as teaching hospitals not affected by workhour limits. This study does a better job of telling us "this is the way it is" than "why is it this way"?
Our results suggest that unintended consequences of resident work hour limits may have occurred in teaching hospitals only. Possibly, more technical errors during procedures (APL) are occurring as surgical trainees have fewer hours with which to become technically proficient during their training. In addition, the increased number of shifts made necessary by shorter work schedules may increase the number of informational exchanges by caregivers; this scenario might lead to higher rates of postoperative PEDVT if appropriate and timely antithrombotic measures are not communicated and instituted.Conversely one could also argue that accidental punctures/lacerations would increase with increased fatigue. More study, as they say, is required. Several issues are brought up in the discussion (the paper was presented at the Southern Surgical Association meeting):
Dr. Josef E. Fischer (Boston, Massachusetts): I would like to congratulate the authors for addressing this issue from the standpoint of surgical training programs because heretofore all of the data that we have seen have been from either single institutions or have been associated with medical programs.
I think you are all aware of the fact that recently in the New England Journal of Medicine, Czeisler and his group from Brigham and Women's Hospital published a paper concerning medical ICU with the interns that seemed to have less than adequate supervision and the number of errors they made after a certain period of time on duty.
I was interviewed for the Wall Street Journal by Laura Landrau, who is one of the very well-respected assistant managing editors, and pointed out to her that I thought that the authors had a vested interest and a conflict, basically because all of the previous work was based on the fact that there was such a problem, and that I thought what the outcome really reflected was the fact that, in a largely unsupervised medical ICU setting with a raw, new medical intern, this was an expected outcome without senior supervision and that in a surgical service in which there is senior supervision at most or all times, the results might be different.
Unfortunately, the only thing that was quoted of our fairly long interview was the fact that I thought that 90 to 92 hours was a necessary period of time for continuity of care, and this is the result of the studies that Bob Bower carried out in Cincinnati, and that was our data. I got into a fair amount of trouble with that quote in the People's Republic of Massachusetts, which seems to be somewhat different from the rest of the country.
And yet this paper, I think, asks several cogent questions. But I have a little difficulty with the parameters such as those chosen because I think the basic issue, at least for a surgical service, is continuity of care. And, I have difficulty, as does Dr. Bland, transposing continuity of care into the observed outcome.
So my questions for the authors are: Are there other parameters that are more closely linked to continuity of care? Or are there other questions that the authors asked that were not particularly answered by the types of parameters that were chosen? Because I think certainly for a surgical service, continuity of care is the basic issue, an issue that is still out there and needs to be answered.
That paper was discussed here. And this is a point I have made repeatedly concerning the 80-hour workweek:
Dr. Thomas R. Gadacz (Augusta, Georgia): There are several issues about the 80-hour work week. First, the 80-hour work week is mandated for all residency training programs. Second, what is an 80-hour work week and how are those 80 hours spent? Can we have an 80-hour plus work week and structure it so that patient care is not fragmented and fatigue and medical errors avoided? Third, what work effort can residents expect once they enter practice?
Although we haven't analyzed all the data, we are completing a survey from the Southeastern Surgical Congress on the work hours of physicians in practice. A real surprise is the finding that the mean average work hours of surgeons in full-time practice is around 65 hours per week, and 20% of the surgeons in practice exceed 80 hours. I would be very surprised if that is going to change just because the 80-hour work week has been mandated for residents. Surgery residents going into practice may have to work longer than 80 hours per week.
We need to design a work hour week that is not totally dependent upon total hours and allow sufficient rest to prevent impairment because of sleep deprivation. Surgeons in practice seem to have better control of their hours to avoid exhaustion. We need to design systems within the residency program that can control the fatigue component and simply not just focus on the 80-hour work week.[emphasis mine]
More to come, I'm sure. |
Tuesday, June 07, 2005
Grand Rounds XXXVII....
It's graduation time at MedGadget. Please refrain from throwing around a beach ball or blowing an air horn, please. |
It's graduation time at MedGadget. Please refrain from throwing around a beach ball or blowing an air horn, please. |
Sunday, June 05, 2005
I Sense Great Fear in You.....

You were destined to have a Red Lightsaber.
Red is the color of fire and blood, so it is
associated with energy, war, danger, strength,
power, and determination as well as passion and
desire. You have seen the Strength and Power of
the Dark Side of the Force and have you thirst
for more of it.
What Colored Lightsaber Would You Have?
brought to you by Quizilla
H/T to Orac |

You were destined to have a Red Lightsaber.
Red is the color of fire and blood, so it is
associated with energy, war, danger, strength,
power, and determination as well as passion and
desire. You have seen the Strength and Power of
the Dark Side of the Force and have you thirst
for more of it.
What Colored Lightsaber Would You Have?
brought to you by Quizilla
H/T to Orac |
Saturday, June 04, 2005
Scrub Fashion.....
Bouncing around I came across this post from Maria offering advice on scrub couture:
There's more:
My training program wasn't one of the ones that were strict about scrubs outside the OR. So when I started my internship I and the other intern loaded up on scrubs and wore them all the time. They then purchased a "scrub ATM" to control loss. Your "account" had three sets of scrubs in it. You would "withdraw" a pair and "deposit" it when you were done. It was very high tech with a camera to make sure you actually deposited scrubs. We were told that if seen in "old scrubs" we could get into trouble. We simply got around it by depositing the pants of a set, getting a full set, then depositing the shirt of a set and getting another. It was delightful on the last day of my residency to deliver a hefty bag full of scrubs to the OR manager that I had worn for the past five years.
BTW I have discovered that a dark t-shirt is best under scrubs since Hibiclens (an antiseptic soap used as a surgical scrub) can stain clothes. |
Bouncing around I came across this post from Maria offering advice on scrub couture:
If you are a man, wear a shirt underneath your scrub top. There is nothing sexy about your scraggly chest hair sprouting forth in all directions for all to see. It does not augment any virility (or lack there of) you may already have. Contrary to what you may think, this unkempt appearance does not overwhelm women with the desire to sidle up to you and run our fingers along your chest. We actually laugh at you.What, you don't dig the Brillo Pad look?
There's more:
Err towards wearing scrub pants one size too large, particularly if you are man. Especially if you’re the type of fellow who lounges in chairs, hands behind your head, legs splayed wide open in an effort to occupy the greatest area possible of the seat supporting you. The general hospital population has little to no interest in what underlies those miniature pant legs as they creep up your calves. We also don’t particularly want to know the circumference of your thighs or the size of your sexual endowment, no matter how greatly you (subconsciously?) wish to advertise such information. (See “wear a shirt underneath your scrub top”.)
My training program wasn't one of the ones that were strict about scrubs outside the OR. So when I started my internship I and the other intern loaded up on scrubs and wore them all the time. They then purchased a "scrub ATM" to control loss. Your "account" had three sets of scrubs in it. You would "withdraw" a pair and "deposit" it when you were done. It was very high tech with a camera to make sure you actually deposited scrubs. We were told that if seen in "old scrubs" we could get into trouble. We simply got around it by depositing the pants of a set, getting a full set, then depositing the shirt of a set and getting another. It was delightful on the last day of my residency to deliver a hefty bag full of scrubs to the OR manager that I had worn for the past five years.
BTW I have discovered that a dark t-shirt is best under scrubs since Hibiclens (an antiseptic soap used as a surgical scrub) can stain clothes. |
Friday, June 03, 2005
The Surgeon as Technician......
Orac unleashes his disdain on a comment to this post at Pharyngula which reads:
So I am technical, but not a technician. |
Orac unleashes his disdain on a comment to this post at Pharyngula which reads:
Surgeons and other medical staff are the equivalent of technicians, engineers, plumbers or carpenters. They are not scientists. They are not studying the details of the relevant science. They don't have to understand it - just carry out procedures by rote. Though the ones who do have a clue will be a lot better at adapting to new circumstances because they'll make more correct guesses based on their understanding than the clueless ones will.This is a misperception that surgeons have had to deal with since they stepped out of the barbershop. Surgery is much more than just operating. Orac puts forth the old piece of surgical wisdom:
We have a saying in surgery: "You can teach a monkey to operate; you just can't teach a monkey when to operate or who needs what operation--or what to do if things are not what expected."Or as one of my attendings would tell us :Operating is easy, surgery is hard.The decision to operate requires a knowledge of anatomy, physiology, pathology, biochemistry,ect...because if you don't you are likely to end up with a dead patient. Operations have consequences, and a surgeon needs to know what they might be so that they may be addressed.
So I am technical, but not a technician. |
Wednesday, June 01, 2005
Tales from the Operating Room VI....
Or: "How the Simple Things Can be a Challenge"
A teenager in remission from lymphoma. The infusaport has been in place for over a year and has not been accessed in over 4 months. It was placed at another facility via a left subclavian approach. The local pediatrician who had assumed care sent the patient to me for removal.
All was going well. I cut down on the "button", dissected it out, and removed the catheter. No resistance was met. Imagine my surprise when I examined the specimen:

That looks a little short to me. Brought in the C-arm and looky here:

Proximal and distal ends marked. Since the preferred approach is now endovascular I closed the wound. Here is a CXR obtained before going to the angio suite:

Ends again marked. Some images from the endovascular attempt:
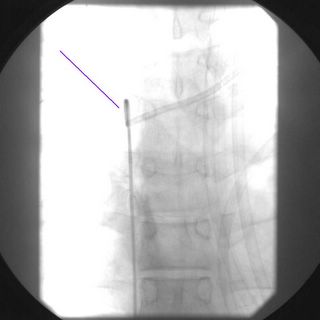
A catheter from a femoral approach. Multiple attempts were made with a snare to grab the distal end.
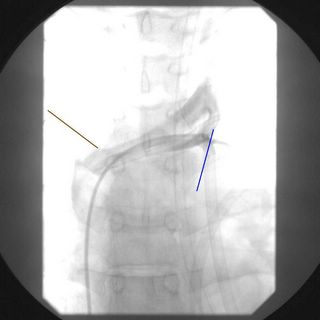
Attempts made to grab proximally. Contrast from a venogram can be seen. The radiologist estimates that about 1-2 cm of the catheter is extraluminal. The catheter seems to be held in place by a fibrin sheath. I review the images with a thoracic surgery colleague who felt that a cutdown approach to retrieve it would be possible. With by thoracic surgeon as a backup off we go.
Using c-arm I localize the catheter and cut down on it. Split the pectoralis major. Cell layer by cell layer divided with frequent re-checks of the flouroscopy to make sure it does not migrate. Eventually I found it and out it comes:

The postop CXR:

How did this happen? A phenomenon known as "Pinch off Syndrome" has been described with subclavian catheters. It has to do with the anatomy of the space between the clavicle and first rib, as seen here:
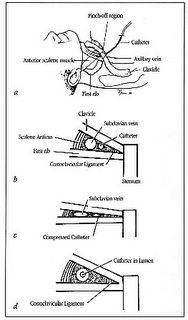
The particular placement of this catheter also contributed:
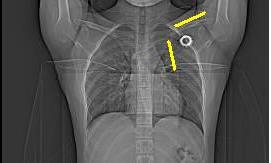
(You may need to zoom in). The top yellow line represents the superior curve and the lower yellow line represents where the catheter enters the costoclavicular space at almost a right angle. The catheter portions were crimped at that site. The catheter had probably been divided for a while. Yet another reason that I do not like subclavian placement of long-term catheters |
Or: "How the Simple Things Can be a Challenge"
A teenager in remission from lymphoma. The infusaport has been in place for over a year and has not been accessed in over 4 months. It was placed at another facility via a left subclavian approach. The local pediatrician who had assumed care sent the patient to me for removal.
All was going well. I cut down on the "button", dissected it out, and removed the catheter. No resistance was met. Imagine my surprise when I examined the specimen:

That looks a little short to me. Brought in the C-arm and looky here:

Proximal and distal ends marked. Since the preferred approach is now endovascular I closed the wound. Here is a CXR obtained before going to the angio suite:

Ends again marked. Some images from the endovascular attempt:
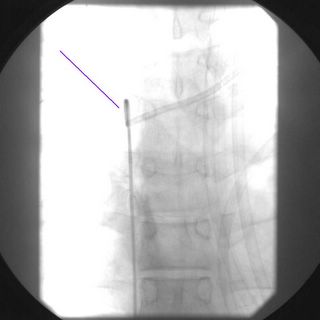
A catheter from a femoral approach. Multiple attempts were made with a snare to grab the distal end.
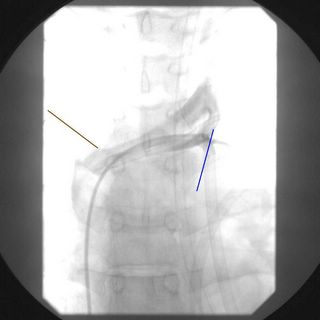
Attempts made to grab proximally. Contrast from a venogram can be seen. The radiologist estimates that about 1-2 cm of the catheter is extraluminal. The catheter seems to be held in place by a fibrin sheath. I review the images with a thoracic surgery colleague who felt that a cutdown approach to retrieve it would be possible. With by thoracic surgeon as a backup off we go.
Using c-arm I localize the catheter and cut down on it. Split the pectoralis major. Cell layer by cell layer divided with frequent re-checks of the flouroscopy to make sure it does not migrate. Eventually I found it and out it comes:

The postop CXR:

How did this happen? A phenomenon known as "Pinch off Syndrome" has been described with subclavian catheters. It has to do with the anatomy of the space between the clavicle and first rib, as seen here:
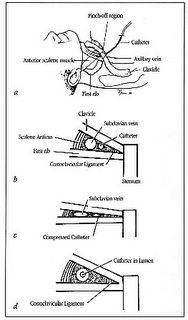
The costoclavicular space. Anatomic (a) and diagrammatic (b) representations. If the catheter passes through the areolar tissue of this space outside the vessel lumen (a medical insertion), it is vulnerable to compression by the clavicle and first rib. (c) Repeated compressive and shearing forces act on the catheter as the shoulder is raised and lowered. (d) A more lateral insertion of the catheter allows it to travel within the subclavian vein. This vessel lies in a more capacious region, and thus by geometric considerations it is protected from compression.
The particular placement of this catheter also contributed:
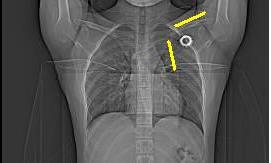
(You may need to zoom in). The top yellow line represents the superior curve and the lower yellow line represents where the catheter enters the costoclavicular space at almost a right angle. The catheter portions were crimped at that site. The catheter had probably been divided for a while. Yet another reason that I do not like subclavian placement of long-term catheters |
Killer on the Road...
Busy days for ED's, trauma surgeons, and unfortunately coroners in Georgia this past weekend. From the Atlanta Journal-Constitution:Traffic deaths set record for holiday
Wear your seatbelts!!! |
Busy days for ED's, trauma surgeons, and unfortunately coroners in Georgia this past weekend. From the Atlanta Journal-Constitution:Traffic deaths set record for holiday
This was the deadliest Memorial Day weekend on Georgia roads since authorities began keeping track 36 years ago.
By Monday evening, 35 traffic deaths had been reported to the Georgia State Patrol, breaking the Memorial Day weekend record of 27 set in 1969, when record-keeping began.
The dead included four members of an Atlanta family, a 15-year-old girl and three Loganville men.
Rain-slicked roads, speed, alcohol and failure to wear seat belts contributed to the death toll for the weekend, which began at 6 p.m. Friday.
Fourteen traffic deaths occurred in metro Atlanta, including two Monday afternoon in Cherokee County, authorities said.
In Gwinnett County, a 15-year-old girl was killed early Monday when the car driven by her 16-year-old brother ran off the road near Lawrenceville. The boy and a 13-year-old sister survived. Both were wearing seat belts, police said. However, the sister who died was not buckled in, said Gwinnett police Cpl. Darren Moloney.
Authorities did not release the names of the teenagers but said the boy had been speeding.
Speed was also blamed for a death about eight hours later in DeKalb County. The driver lost control on Flakes Mill Road and crossed into a lane of oncoming traffic, said DeKalb police Officer Cory Hughes. A passenger in the car, 29-year-old Dayonne Wilson of Ellenwood, was killed.
Several wrecks involved multiple fatalities. Four people, all members of the same Atlanta family, were killed Sunday morning when their vehicle struck a tree in Greene County. Michael Carter, 35, his wife, Almeda Rawlings, and two other family members were returning from Myrtle Beach, S.C., when their car ran off I-20 at 6:55 a.m., said county Coroner Steve McCommons.
Three men died Saturday afternoon in Loganville when their pickup truck ran off the road and struck a tree, said Walton County Coroner Craig League.
In the week leading up to Memorial Day, the Governor's Office of Highway Safety filled the airwaves with messages aimed at persuading people to buckle their seat belts. The messages also warned that troopers would be watching for speeding drivers.
"I don't know if it didn't work this year or whether luck was on their side in past years," said Trooper Larry Schnall, a spokesman for the Georgia State Patrol. "The most common response that I hear from people is that they feel like it won't happen to them."
Every holiday weekend, the patrol issues traffic wreck predictions to encourage people to drive safely. For this Memorial Day period, the agency had predicted 2,550 wrecks, 650 injuries and 17 deaths.
By the end of the holiday period, 2,726 wrecks had been reported, resulting in 830 injuries and 35 deaths.
Wear your seatbelts!!! |







