Thursday, July 13, 2006
Tales From the Operating Room X.....
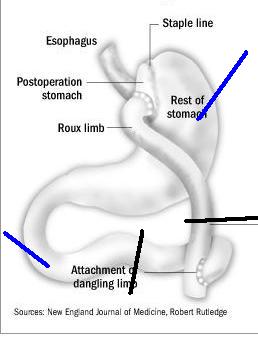
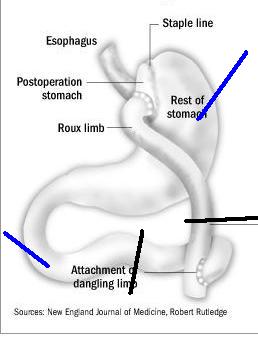
Or when gastric bypass is not your friend. Young patient several years out from laparoscopic gastric bypass presents with severe abdominal pain. Over the past several weeks they have had intermittent attacks of pain which lasted only a few minutes. This episode did not resolve and they were diagnosed with a small bowel obstruction. The patient underwent nasogastric decompression, a not too effective maneuver as you see here:

The black line represents the NG tube. With the majority of the stomach and small bowel excluded (red) the only area that can be decompressed is seen in blue. A few hours later the patient developed hypotension and I was called to evaluate the patient. They had guarding and rebound on abdominal examination. Off to the OR. Gross pictures follow.
[
[
[
[
[
[
[
[
[
[
[
[
[

The yellow circle represents the jejunal anastamosis. Here is another view.

The yellow circle indicates the transverse colon. Obviously this bowel is severely ischemic. The vast majority of the small bowel will need to be removed. How did it become so? It was due to an internal hernia posterior to the bypass limb. The area in question is indicated by the black circle.

The hernia was reduced and the bowel irrigated with warm saline, we spoke softly to it and used flourescin and a Woods lamp, but to no avail. The small bowel from the ligament of Treitz to the terminal ileum was removed. About a third of the roux limb was also removed. By my crude measurements this left about 50 cm of small bowel en vivo. The cecum was marginal but the length of small bowel needed is reduced if the ileocecal valve is intact. A gastrostomy and duodenostomy were placed to allow for decompression.
The black lines represent the resection lines and the blue lines represent the locations of the tubes. The patient was acidotic and hypothermic so the procedure was abandoned to allow for resuscitation in the ICU and a second look in 24 hours.
They required all sorts of blood products but by morning the patient was out of shock and ready for the return trip.
Which was disappointing.
The marginal terminal ileum and cecum were necrotic, as was another third of the roux limb. This left them with about 25-30 cm of small bowel. The end of the roux limb was exteriorized as an ostomy.
The patient recovered and shortly before discharge I placed a port for TPN. I saw the patient back in the office the other day and they are doing as well as can be expected. Now we have to send them off for additional surgery to restore continuity of the bowel.
Oh, and since this was a complication from a non-covered procedure, their insurance is not paying for any of this. Not the hospital, not my fees, not the home TPN. |
Or when gastric bypass is not your friend. Young patient several years out from laparoscopic gastric bypass presents with severe abdominal pain. Over the past several weeks they have had intermittent attacks of pain which lasted only a few minutes. This episode did not resolve and they were diagnosed with a small bowel obstruction. The patient underwent nasogastric decompression, a not too effective maneuver as you see here:

The black line represents the NG tube. With the majority of the stomach and small bowel excluded (red) the only area that can be decompressed is seen in blue. A few hours later the patient developed hypotension and I was called to evaluate the patient. They had guarding and rebound on abdominal examination. Off to the OR. Gross pictures follow.
[
[
[
[
[
[
[
[
[
[
[
[
[

The yellow circle represents the jejunal anastamosis. Here is another view.

The yellow circle indicates the transverse colon. Obviously this bowel is severely ischemic. The vast majority of the small bowel will need to be removed. How did it become so? It was due to an internal hernia posterior to the bypass limb. The area in question is indicated by the black circle.

The hernia was reduced and the bowel irrigated with warm saline, we spoke softly to it and used flourescin and a Woods lamp, but to no avail. The small bowel from the ligament of Treitz to the terminal ileum was removed. About a third of the roux limb was also removed. By my crude measurements this left about 50 cm of small bowel en vivo. The cecum was marginal but the length of small bowel needed is reduced if the ileocecal valve is intact. A gastrostomy and duodenostomy were placed to allow for decompression.
The black lines represent the resection lines and the blue lines represent the locations of the tubes. The patient was acidotic and hypothermic so the procedure was abandoned to allow for resuscitation in the ICU and a second look in 24 hours.
They required all sorts of blood products but by morning the patient was out of shock and ready for the return trip.
Which was disappointing.
The marginal terminal ileum and cecum were necrotic, as was another third of the roux limb. This left them with about 25-30 cm of small bowel. The end of the roux limb was exteriorized as an ostomy.
The patient recovered and shortly before discharge I placed a port for TPN. I saw the patient back in the office the other day and they are doing as well as can be expected. Now we have to send them off for additional surgery to restore continuity of the bowel.
Oh, and since this was a complication from a non-covered procedure, their insurance is not paying for any of this. Not the hospital, not my fees, not the home TPN. |






