Monday, October 04, 2004
The Future of Surgery II...
Continuing the discussion of this article from the October 2004 Annals of Surgery: Surgical Education in the United States: Portents for Change. This post will discuss the changes in surgical education on medical students, residents, and academia. First the students:
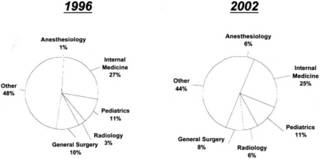
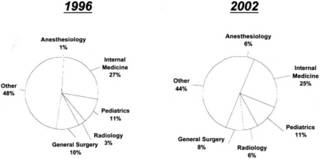
Medical school career choices, ranking specialties, 1996 vs 2002:
As for the residents:
Now to academia:
The final post will concern general and specialist surgeons.Cross-posted at Galen's log
Continuing the discussion of this article from the October 2004 Annals of Surgery: Surgical Education in the United States: Portents for Change. This post will discuss the changes in surgical education on medical students, residents, and academia. First the students:
For medical students, surgery has become an increasingly unappealing area of medical practice. The National Residency Matching Program suggests that from 1992 to 2000, the numbers ranking general surgery as a preferred discipline fell from 1950 to 1500, an overall decrease of approximately 23%. For US seniors, the fall has been more dramatic, on the order of 36%. The only increase has been in US citizens educated in international medical schools. This number reached a maximum of 140 individuals as of 2002 and, although its overall impact is limited, the impact in terms of the quality of applicants for surgical programs is real. An increase in international medical graduates can compensate for this shortage, but it has inherent problems in terms of the difficulty in evaluating foreign graduate medical education and increasing immigration service review of foreign access to US surgical programs. Active programs to improve international medical graduate performance are currently under way.The NRMP data may be found here on page four. While the trend has improved somewhat, surgery has not regained the popularity it once had.
Students shun the rigors of surgical training and view the profession as too demanding and providing little opportunity for personal time. From 1996 to 2002, controllable lifestyle explained 55% of variability in specialty preference, controlling for income, work hours, and years of graduate medical education. Medical student choices have changed to user-friendly specialties. Currently, the median debt at completion of medical school is over $100,000 . Over 25% of medical school graduates of 2002 incurred a debt greater than $150,000.13 The prolonged length of surgical training, fellowship, and research experience, requiring 9 to 11 years post-MD at subsistence pay, is poorly perceived, and a strong belief that years are wasted in service without education is a strong disincentive.So based on the above, over half of medical students based their specialty choice on the perceived control over lifestyle. Needless to say, general surgery is not well known for having a "controllable lifestyle". That is not likely to change even with "reforms". Such specialties as anesthesia, radiology, and emergency medicine have excellent lifestyle control mechanisms. Surgery residency is already five long years with some programs requiring more time, and with workhour limits, it may grow even longer. Not exactly a move that will suck the medical students in.
Medical school career choices, ranking specialties, 1996 vs 2002:
A powerful factor in the choice of medical specialty is identification with role models. Role models are the impetus to entry into a surgical subspecialty in 56% of residents. What makes an ideal role model has been debated and defined Role models can be introduced at any point in a training program, perhaps best in medical school. How well do we as surgeons match up to the important attributes that emphasize, as in internal medicine, dedicated time as a teacher, doctor-patient relationships, the teaching of psychological aspects of care, and prior chief resident experience?Surgeons match up pretty poorly when compared with other specialties in reference to "dedicated time as a teacher, doctor-patient relationships, the teaching of psychological aspects of care". It probably has to do with the personality types that migrate into surgery. Want examples? Look at this post comparing the "pimping" styles of internists and surgeons.
As for the residents:
Whether surgeons of our vintage appreciate it or not, an inescapable change has taken place in today's residents with respect to their perceived needs for a balanced lifestyle that allows more time with families and free time to follow their interests. We dismiss the lifestyle needs of residents at the peril of our recruitment success.Give the NRMP data, postgraduate surgical education has become a "buyers market".
Over the years, residents have accumulated more and more administrative chores, many of which make little sense in an environment that is so rich in information systems. Processes by which patients are admitted, cared for, and discharged are antiquated, take minimal advantage of information technology, and impose an unjustifiable burden on residents. These processes need to be totally revised and adapted to current needs. Surgical education has to be more about understanding, imagination, and communication as well as training and skill acquisition. Surgical training programs are perceived as being none of these, but rather focused on service delivery, particularly to the poor and underprivileged. At present, 20% of surgical residents taking the American Board of Surgeons Qualifying examination are female, whereas females constitute 50% of the medical school graduates. The overall contribution of women to the long-term workforce in surgery is limited appropriately by the desire and need for a lifestyle that can accommodate childbearing and childrearing without limiting professional satisfaction. Few residencies have innovative programs to address the important need of women residents and that of male-resident fathers whose spouses have a full-time professional career. The desire for women to enter surgical subspecialties is variable, with increases in female orthopaedic residents lagging behind increases in other areas. We need to recognize that many medical students approach residency together as a couple, requiring adaptability in the residency match. How well can we adapt to this 2-person professional medical family?How well surgical education adapts to these issues will determine the future of the practice of general surgery.
To compound this perception of too little time to learn too much, we impose volume requirements for each resident that are difficult, if not impossible, to meet. The extensive clinical spectra to be covered by any one resident make any proposed decrease in the length of training difficult. We have been reluctant to acknowledge that most institutions and residencies cannot provide the volume and breadth of clinical material that we demand they be exposed to!I agree. I remember readying myself for the boards, both written and oral, and having to review a good deal of head and neck surgery. I had done maybe 2 radical neck procedures. This is one reason that the American Board of Surgery has initiated an Early Specialization Program . This allows those wishing to pursue specialization in pediatric or vascular surgery to reach their goal 1 year earlier than planned. Some programs also exist for plastic surgery and maybe soon in thoracic surgery.
The resident facing his board examinations may be justified in complaining when he or she is examined in technical aspects of pancreatic, esophageal, or infected aorto-iliac graft surgery that he or she has rarely seen and never performed.
Now to academia:
Teaching can impose a degree of inefficiency in the provision of hospital services, and typically the cost structure of teaching hospitals is 25% to 30% higher than that of community hospitals. Thus, hospitals will scrutinize and demand appropriate reimbursement for the cost of this necessary inefficiency if they are to survive in an arena of brutal health market competition.In the modern era of evidence based medicine and efficiency, the academic medical center operates at a severe disadvantage. Turnover in departments is increasing as the emphasis moves from teaching to production.
Faculty in medical schools already demonstrate a 30% level of high emotional exhaustion and burnout, with younger surgeons more affected! Given the current faculty workload of between 60 and 80 hours per week, it is unlikely they can absorb more teaching and clinical cases. Exhausted faculty are poor role models!
Residency programs are the pride of academic surgical departments and provide the single most important focus for faculty unity. As reimbursements for physician services decline and faculty work longer hours and cope with increasing documentation, their ability to devote adequate time to teaching and other scholarly activities has been strained. Most departments do not make specific financial commitments for teaching. It is fortunate that faculty members receive gratification from teaching and their association with residents in the care of sick patients. The lack of specific compensation for teaching will in the long term degrade the learning environment and challenge the traditional ad hoc understanding under which surgical education is provided. How and by whom should surgeons be financially compensated for the teaching they do? How will we accept that the process of education is an equally fruitful source of research and evaluation? A desirable pathway to surgical fulfillment is currently poorly recognized and inadequately compensated.
The final post will concern general and specialist surgeons.Cross-posted at Galen's log
Labels: Future of Surgery
|





