Wednesday, January 17, 2007
Castro Colon Conjecture......
A great deal in the news the past few days about Cuban dictator Fidel Castro's recent encounter with his country's socialist utopian medical system. One piece of information making the rounds is that El Jefe himself ruled out a colostomy.
While all of what is out there is rumor, Castro sounds as if he has experienced one of the great joys of abdominal surgery, an enterocutaneous fistula:
As well as "bile duct inflammation":
Regardless, it is doubtful we will ever know how Castro ended up this way.
A great deal in the news the past few days about Cuban dictator Fidel Castro's recent encounter with his country's socialist utopian medical system. One piece of information making the rounds is that El Jefe himself ruled out a colostomy.
Fidel Castro himself told surgeons not to perform a colostomy, opting instead for a course of surgery that produced a complication that left the Cuban leader in far worse condition, according to a newspaper report Wednesday.Imagine the conversation, Castro surrounded by his medical team and surgeons:
After removing an inflamed piece of Castro's large intestine in an operation last year, the doctors connected the remainder directly to his rectum, rather than attaching a colostomy bag, El Pais said, quoting two medical sources at Madrid's Gregorio Maranon hospital. The operation failed when a suture burst.
"The Cuban dictator and his advisers are the ones who decided on the surgical technique that has led to the complications," the paper said.
SURGEON #1: El Presidente, we must remove your colon due to the inflammation. The safest way to do so would be to remove the diseased portion and leave a colostomy.
CASTRO: No. No colostomy. Chicks don't dig the bag.
SURGEON #1: But Maximum Leader.....
CASTRO: Take him away. (Surgeon #1 take out of room, never to be seen again.)
CASTRO (to surgeon #2): What do you think?
SURGEON#2: No colostomy, understood Jefe!!!
While all of what is out there is rumor, Castro sounds as if he has experienced one of the great joys of abdominal surgery, an enterocutaneous fistula:
El Pais said that in December, when Garcia Sabrido visited, Castro had an abdominal wound that was leaking more than a pint of fluids a day, causing "a severe loss of nutrients." The Cuban leader was being fed intravenously, the report said.
As well as "bile duct inflammation":
“In the summer, the Cuban leader bled abundantly in the intestine,” El Pais reported. “This adversity led him to the operating table, according to the medical sources. His condition, moreover, was aggravated because the infection spread and caused peritonitis, the inflammation of the membrane that covers the digestive organs.”I have also read that the "Spanish stent" was some sort of "experimental artificial bowel" or some such other. The coverage also seems to use the term "diverticulitis" in both the usual medical sense and also to mean "diverticulosis" as well. The reports of intestinal bleeding seem to go along more with the diagnosis of diverticulosis, than diverticulitis. But there is also mention of "infection spread" and "peritonitis", terms more consistent with diverticulitis. Intractable bleeding from diverticulosis is treated with surgery if other measures fail. Because blood in the bowel serves as a cathartic, and there is no evidence of infection, the argument for primary repair can be made. In an 80-year old, especially one who has had multiple transfusions and may be in shock, a Hartmann's Operation would be my procedure of choice. In the case of diverticulitis, depending on the amount of contamination, some advocate primary repair and the use of on-table colonic lavage.
The recovery from the first operation, in which part of his large intestine was extracted and the colon was connected to the rectum, did not go well. The link broke and he released feces into the abdomen that caused another peritonitis, the report said.
A second operation to clean and drain the infected area also failed, the paper said. He was then hit with inflammation of the bile duct, an illness which has a 80 percent mortality rate, el Pais said. A prosthesis made in South Korea was implanted and failed and later was replaced with one made in Spain.
Regardless, it is doubtful we will ever know how Castro ended up this way.
Labels: celeberty medicine, colon, Fidel Castro, surgical complications
|Tuesday, January 16, 2007
Georgia Trauma System Update.....
From Peach Pundit and the Macon Telegraph comes the latest on the funding for the long-overdue state-wide trauma system. Some advice: slow down.
The problem:
The devil, as always, is in the details:
Between this and CON, it makes for an interesting session.
From Peach Pundit and the Macon Telegraph comes the latest on the funding for the long-overdue state-wide trauma system. Some advice: slow down.
The push is on to find new sources of revenue to improve the state's trauma network, and it may lead to big new fines for speeders.Mr. O'Neal's brother, BTW, is the State EMS Medical Director here in Georgia. Dr. O'Neal has done a fine job here in Georgia and has been a tireless advocate for trauma system development here in Georgia.
Gov. Sonny Perdue has announced a plan to tack on "additional, substantial fines" for so-called "superspeeders," Perdue press secretary Bert Brantley said. That money would be used to improve emergency care in rural Georgia and give a boost to hospitals that lose money caring for severely injured people.
Other ideas to fund improvements are also percolating at the Capitol, and a finished bill - or bills - may be weeks away from debate. The governor's office hasn't set the amount of the new fine, but Brantley said it would be "potentially in the hundreds of dollars."
Two midstate lawmakers are heavily involved in the process, having co-chaired a study group on trauma-care issues this summer.
State Sen. Cecil Staton, R-Macon, and state Rep. Larry O'Neal, R-Warner Robins, said Perdue's plan will have to be discussed. Both men are working on bills to create a permanent commission to manage funds set aside for improvements and keep an eye on the issue after it fades from the limelight of this General Assembly session.
The problem:
The problem is the need to quickly treat severely injured people - and the high cost of doing so. Surgeons must be kept on call, expensive equipment must be on hand, and the injured person must be transported quickly.
That's difficult, particularly in rural Georgia, where there are large gaps in the state's network of hospitals equipped to handle the most serious injuries. In fact, the study group found that Georgia's trauma death rate is 20 percent above the national average - a difference of about 700 lives a year.
Money is a big part of the reason. Of the state's 152 acute-care hospitals, 15 are designated trauma centers. And four - in Macon, Atlanta, Augusta and Savannah - offer the highest level of care, the report states. Many hospitals don't offer these services, in part, because of a high level of uninsured patients seeking care, the report states.
Doctors, hospitals and EMS services lose about $250 million a year on trauma care, the report states. The Medical Center of Central Georgia in Macon has complained of this in the past, saying shortfalls could lead the hospital to drop its level of care.
The devil, as always, is in the details:
The answer, according to several legislators, is to develop a new pool of money to establish new trauma centers, keep the current ones solvent and purchase more helicopters to quickly transport accident victims, who would receive free transport.
Increasing speeding fines would require a constitutional amendment, which in turn would require a statewide referendum, O'Neal said. O'Neal said he would probably support increased fines for "superspeeders," but to expect intense debate over just what that means.
For the moment, the governor's office has defined a "superspeeder" as anyone who drives faster than 85 mph, or 75 mph on a two-lane road, Brantley said. The governor's proposal also targets habitual violators who lose their driver's license and would pay a heavier fine when they reapply for the license, Brantley said.
Staton said he's glad to have the governor on board, but both he and the governor's office agree that new fines might not raise enough money. Projections have put the initial cost of the trauma network need at $85 million, with a lower cost recurring each year.
The study group's report also listed several funding options besides new traffic fines, including:
• Diverting a portion of the Georgia insurance premium tax.
• A $5 surcharge on motor vehicle registrations.
• A $1.16 monthly surcharge on cell phones.
• Surcharges on rental and leased cars.
• An option on Georgia tax forms allowing people to donate a portion of their tax refund to the trauma care fund.
Because the changes would also help prepare the state for a large-scale disaster, O'Neal said he's hoping federal money will be available through homeland security grants.
The ball is rolling on the issue, and there seems to be enough support to make significant changes, Staton said.
The question is "what the numbers will ultimately be," he said.
Between this and CON, it makes for an interesting session.
Labels: Georgia, Trauma System Development
|
Grand Rounds Vol. III No. 17.......
Hosted in a poetic format this week by Six Until Me.
Hosted in a poetic format this week by Six Until Me.
Labels: Grand Rounds
|Monday, January 15, 2007
More on the Future of Surgery......
Dr. Schwab has a post about his experience as an acute care surgeon (ACS) or a "surgical hospitalist". I have posted about this several times before (just click on the "future of surgery" tag). Dr. Schwab agrees that the acute care surgeon will have a role to play in the future. How and why? Let us count the ways:
1. The 80-hour work limits have exposed current trainees to five years of very predictable schedules, night floats, and guaranteed time out of the hospital. The ACS model fits this paradigm quite well.
2. With over 3/4 of current residents going on for further fellowship training having someone who can emergently "stop the bleeding and drain the pus" without much delay will be needed.
3. Hospitals will need a reliable cadre of surgeons who can provide emergency room coverage.
Dr. Schwab shares the opinion that objections will be raised by some because "it cuts into their gig" I think that objection is overcome by what I have called the "briar patch effect" of ACS:
Dr. Schwab and his group have,IMHO, done it the right way with an estblished group bringing somebody in to allow the other surgeons to be in the OR making money.
Stronger objections will concern the "ownership" of the surgical patient, how the acture care surgeon relates to his "somnolent elective" colleauges, and the possibility that acute care surgeons will be considered a "surgical underclass". No matter how many curricula, meetings, or fellowships they may come up with, how the ACS system addresses these will determine the fate of the acute care surgeon.
Dr. Schwab has a post about his experience as an acute care surgeon (ACS) or a "surgical hospitalist". I have posted about this several times before (just click on the "future of surgery" tag). Dr. Schwab agrees that the acute care surgeon will have a role to play in the future. How and why? Let us count the ways:
1. The 80-hour work limits have exposed current trainees to five years of very predictable schedules, night floats, and guaranteed time out of the hospital. The ACS model fits this paradigm quite well.
2. With over 3/4 of current residents going on for further fellowship training having someone who can emergently "stop the bleeding and drain the pus" without much delay will be needed.
3. Hospitals will need a reliable cadre of surgeons who can provide emergency room coverage.
Dr. Schwab shares the opinion that objections will be raised by some because "it cuts into their gig" I think that objection is overcome by what I have called the "briar patch effect" of ACS:
A popular trend to increase the operative potential of the trauma service is to add nontrauma emergency surgery responsibilities. Although this appears to improve the trauma surgeon's operative experience and job satisfaction, reports thus far have focused on providing general surgery emergency services with limited coverage of vascular and thoracic nontrauma emergencies. Initial enthusiasm for this solution has the potential to be short lived because the majority of these surgical emergencies consist of draining soft tissue infections and excising necrotic gastrointestinal structures. Indeed, it can be argued that the trauma surgeon coverage of these surgical emergencies has a greater effect on the job satisfaction of the somnolent elective surgeon that is relieved of these responsibilities.Emphasis mine.
Dr. Schwab and his group have,IMHO, done it the right way with an estblished group bringing somebody in to allow the other surgeons to be in the OR making money.
Stronger objections will concern the "ownership" of the surgical patient, how the acture care surgeon relates to his "somnolent elective" colleauges, and the possibility that acute care surgeons will be considered a "surgical underclass". No matter how many curricula, meetings, or fellowships they may come up with, how the ACS system addresses these will determine the fate of the acute care surgeon.
Labels: Future of Surgery
|
Expanding the Empire.....
From the Journal-Constitution:Athens medical school just what the doc ordered
The site would be at the soon-to-be vacated Navy Supply Corps School located on some prime real estate in Athens. The site is adjacent to Athens Regional Medical Center.
MCG has already done this with its' nursing school. There is some talk of one day setting up an independant medical school at the Athens site:
From the Journal-Constitution:Athens medical school just what the doc ordered
Forty medical school students will begin attending a joint University of Georgia and Medical College of Georgia campus in Athens in 2009, paving the way for a new health science complex at the state's flagship university, UGA president Michael Adams said this week.
Adams, who gave a State of the University address Thursday, said Friday the collaboration could eventually put as many as 200 medical students in Athens, but he stopped short of saying UGA planned to develop its own medical college.
"What we proposed was a joint trial period," working with Medical College of Georgia, he said. "Nobody has committed to anything beyond that."
The site would be at the soon-to-be vacated Navy Supply Corps School located on some prime real estate in Athens. The site is adjacent to Athens Regional Medical Center.
Faculty members from both UGA and MCG will teach at the medical school, which MCG President Daniel Rahn described as a regional campus for the Augusta-based college.
In the past year, MCG has increased enrollment of first-year students from 180 to 190. Adding another 40 students a year in Athens beyond that number will help combat statewide and national physician shortages, he said.
The Association of American Medical Colleges has called for increasing enrollment of medical students by 30 percent by the year 2015 through expanding existing schools and creating new ones. After 20 years of no growth in the number of medical schools, several states, including Florida and Texas, are now building new ones.
Rahn said the Athens campus will be accredited and will use MCG's existing curriculum.
MCG has already done this with its' nursing school. There is some talk of one day setting up an independant medical school at the Athens site:
While no one is speculating publicly on whether the project could morph into a full-scale UGA medical school, the university has been placing an increasing emphasis on healthcare and research. In 2005, UGA opened a College of Public Health and a major center for biomedical and health sciences, and it has been ramping upThere has also been an Osteopathic school opened recently in Georgia.
the university has been placing an increasing emphasis on healthcare and research. In 2005, UGA opened a College of Public Health and a major center for biomedical and health sciences, and it has been ramping up bids for national research dollars. UGA and MCG already have partnerships in nursing and pharmacy programs.
Adams said, of the 10 largest states, Georgia is the only one without three public medical colleges. Currently, Medical College of Georgia is the state's only public medical school. Emory University, Mercer University and Morehouse College run private medical schools.
Labels: Georgia, MCG, medical education, UGA
|Tuesday, January 09, 2007
Grand Rounds Vol 3 No. 16.....
Hosted this week by Dr. John LaPuma. His theme is "Food as Medicine". I agree with Allen that there are good ways and bad ways to do "themed" Grand Rounds. The "good" way in my opinion is to take the posts that are submitted and work them into the "theme" that you choose. Examples can be found here, here and my own example here. A "bad" example can be found here. Nothing against the ChronicBabe or Dr. LaPuma, but the idea of Grand Rounds is to share the best of the medical blogosphere each week. The host gets the increased traffic the week they host, and if the readers like the emphasis of their blog, they can come back. By placing up front restrictions on submissions, the hosts, I believe, do a disservice to the submitting authors.
But since the host's discretion trumps all, I shut up until I can find the time to host again (for the fourth time).
Hosted this week by Dr. John LaPuma. His theme is "Food as Medicine". I agree with Allen that there are good ways and bad ways to do "themed" Grand Rounds. The "good" way in my opinion is to take the posts that are submitted and work them into the "theme" that you choose. Examples can be found here, here and my own example here. A "bad" example can be found here. Nothing against the ChronicBabe or Dr. LaPuma, but the idea of Grand Rounds is to share the best of the medical blogosphere each week. The host gets the increased traffic the week they host, and if the readers like the emphasis of their blog, they can come back. By placing up front restrictions on submissions, the hosts, I believe, do a disservice to the submitting authors.
But since the host's discretion trumps all, I shut up until I can find the time to host again (for the fourth time).
Labels: Grand Rounds, snark
|Monday, January 08, 2007
The Upcoming CON Battle.....
The Georgia General Assembly kicks off today and tort refrom is not the only health-related subject that is up for debate this year. I saw this post from Peach Pundit about the upcoming battle over Certificate of Need (CON) in Georgia a few weks ago and was moved to comment, given the impact that CON will have this year.
For those unfamiliar, a CON is a permit that hospitals and other healthcare institutions must aquire before construction of facilities (even non-medical ones, such as a parking deck) or offer a new service (such as cardiac surgery).
The rationale from the State of Georgia's .Certificate of Need Frequently Asked Questions Review Guide:
There are some projects that are exempt from the CON process:
What has brought this to the forefront was our old friend Dr. Bagnato. Word around the campfire became that Dr. Bagnato's suggested motivation for his lawsuit was Pheobe Putney's opposition to his CON for an ambulatory surgery center. The wrinkle here is that in the state of Georgia general surgery is not considered a single specialty so Dr. Bagnato was not allowed to avoid the CON process.
Dr. Bagnato has found a voice in the Georgia Society of General Surgeons, a group that has been fighting to change the CON laws since its' inception. (Full disclosure, I am not a menber) While I can understand their frustration I do not agree with their reasoning or the protrayal of hospitals.
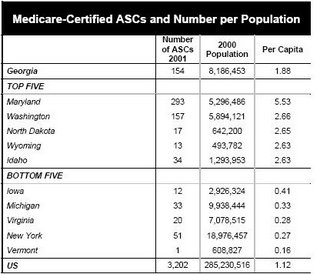
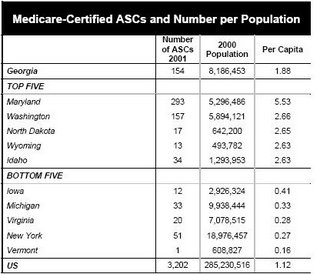
I will be the first to admit my take is skewed by my role in the trauma program in River City, so caveat empetor. I have seen plastic surgeons, ortopedic surgeons, urologists and otolaryngologists stop taking trauma and emergency call because they can do the vast majority of their procedures in office or an ambulatory surgery center (ASC) and not rely on the hospital. EMTALA also places a burden on hospitals (and physicians) that are not shared by the ASC or office-based surgery suites. And despite what may be said, medicine in 2007 is not a free-market system, and the usual rules of supply and demand do not apply. There is some irony that the GSGS supports a statewide trauma network, but is making it more difficult to obtain the coverage needed to make it work (as does the Medical Association of Georgia). We certainly don't lack for ASC's in Georgia as this chart shows we have above the national average per captia number of ASC's:
But the reccommendations are out. For those who wish to read the entire 267 pages of the report, here you go. But for the easily bored, here are the reccommendations from the executive summary that pertain to general surgery and ASC's:
My physician colleagues need to tread carefully here. The hospitals can make a very persuasive argument aimed at the public concerning lack of access to care. If left to their own devices I doubt many of these ASC's will take care of the medically complex or the underinsured. It will be an interesting battle.
The Georgia General Assembly kicks off today and tort refrom is not the only health-related subject that is up for debate this year. I saw this post from Peach Pundit about the upcoming battle over Certificate of Need (CON) in Georgia a few weks ago and was moved to comment, given the impact that CON will have this year.
For those unfamiliar, a CON is a permit that hospitals and other healthcare institutions must aquire before construction of facilities (even non-medical ones, such as a parking deck) or offer a new service (such as cardiac surgery).
The rationale from the State of Georgia's .Certificate of Need Frequently Asked Questions Review Guide:
Georgia’s Certificate of Need Program was codified by the Georgia legislature in 1979 in Georgia's Health Planning Statute, Title 31, Chapter 6. The purpose of the CON program is to insure the availability of adequate health care services to meet the need of all Georgians, while safeguarding against the unnecessary duplication of services that perpetuate the costs of healthcare services. The Department of Community Health was created in 1999 and the administration of the CON Program was placed within the Department.
There are some projects that are exempt from the CON process:
An Ambulatory Surgery Facility that is physician owned, office-based, and single-specialty, the establishment and development of which does not exceed the limited-purpose physician-owned ambulatory surgery centers threshold.According to the footnote the 2004 figure was $1,436,356. The key term above is "single specialty", a term that has generated some controversey.
What has brought this to the forefront was our old friend Dr. Bagnato. Word around the campfire became that Dr. Bagnato's suggested motivation for his lawsuit was Pheobe Putney's opposition to his CON for an ambulatory surgery center. The wrinkle here is that in the state of Georgia general surgery is not considered a single specialty so Dr. Bagnato was not allowed to avoid the CON process.
Dr. Bagnato has found a voice in the Georgia Society of General Surgeons, a group that has been fighting to change the CON laws since its' inception. (Full disclosure, I am not a menber) While I can understand their frustration I do not agree with their reasoning or the protrayal of hospitals.
I will be the first to admit my take is skewed by my role in the trauma program in River City, so caveat empetor. I have seen plastic surgeons, ortopedic surgeons, urologists and otolaryngologists stop taking trauma and emergency call because they can do the vast majority of their procedures in office or an ambulatory surgery center (ASC) and not rely on the hospital. EMTALA also places a burden on hospitals (and physicians) that are not shared by the ASC or office-based surgery suites. And despite what may be said, medicine in 2007 is not a free-market system, and the usual rules of supply and demand do not apply. There is some irony that the GSGS supports a statewide trauma network, but is making it more difficult to obtain the coverage needed to make it work (as does the Medical Association of Georgia). We certainly don't lack for ASC's in Georgia as this chart shows we have above the national average per captia number of ASC's:
But the reccommendations are out. For those who wish to read the entire 267 pages of the report, here you go. But for the easily bored, here are the reccommendations from the executive summary that pertain to general surgery and ASC's:
Recommendation 14.1 (5 Agree, 1 Disagrees, 4 AbstainOn this Dr. Bagnato and I agree. Treat us the same as our orthopedic, urologic, and otolayngologic peers.
Treat General Surgery in a consistent manner as all other single specialties.)
The majority of the Commission recommends that General Surgery be treated in a manner consistent with all other singe specialties, regardless of the regulatory requirement for single specialty facilities.
One member disagrees and maintains that general surgery should be treated as a multi-specialty because of the complex nature of the cases that a general surgeon may perform.
Recommendation 14.2 (5 Agree, 3 Disagree, 2 Abstain)This would allow for ASC's to be built on every street corner if so desired, since need criteria would not be factored into a CON decision. Physicians who utilize an ASC would be required to maintain hospital staff priveledges and take ED call. Another objection, in addition to those described above, is that this would allow hospitals an unfair advantage since if a physician were to resign or be removed from staff, theit CON could be affected. Then there is an absolutist position:
Abolish entirely the exemption for freestanding single specialty, office-based, physician-owned ambulatory surgery centers and require physician-owned limited purpose ambulatory surgery centers to obtain a Certificate from the Department. Upon application, such applicants would not be required to address need criteria but would be required to make indigent and charity care commitments, to accept Medicaid, to supply data to the Department of Community Health, and to verify that all its physicians are members of a hospital staff and are willing to accept emergency room coverage.
The membership of the Commission was sharply divided on the issue of physician-owned single specialty ambulatory surgery centers, which are currently exempt from Certificate of Need if the center can be established for a dollar amount less than approximately $1.6 million. One contingent of the Commission agrees with the recommendation that the current exemption be abolished and that limited-purpose, physician- owned ambulatory surgery centers (“ASC”) obtain a Certificate, although such centers would be free from an objective need methodology. Such ASCs would be required to commit to the provision of indigent and charity care at a level of 3 percent of adjusted gross revenues. In addition, this contingent recommends that these ASCs agree to accept Medicaid, if at all possible, and provide services as a minimum community standard, that such facilities agree to provide annual data to the Department, and that all physicians who perform procedures at the facility be required to hold hospital staff privileges, if possible, and to accept ER coverage. The members who agree with this recommendation do so because freestanding single-specialty ambulatory surgery centers have been shown to be high quality and low cost alternatives. These members who argue for less regulatory control contend that to artificially restrain these services raises costs reduces efficiency, and prevents physicians from billing facility fees.
Other members disagreed with this recommendation and maintain that the exemption for physician-owned ambulatory surgery centers should be abolished and that such centers should be required to obtain a Certificate of Need addressing all applicable review criteria including a determination of need. These members are concerned that if ambulatory surgery centers are allowed to proliferate significantly, hospitals will not have a financially sustainable business model. Mainly, these members maintain that ambulatory surgery centers take low acuity, paying patients, and leave hospitals to treat the complex cases and individuals without the ability to pay.
The CON Commission has been unable to reach consensus with regard to the best policy to address this difficult issue because its root causes involve complex factors relating to reimbursement and costs that are beyond the CON program’s purview. A real and sustainable solution to this dilemma will require a health policy approach that corrects the cost and payment problems for both professional services and hospital-based services, particularly with respect to the under-insured and uninsured.
Recommendation 14.3 (3 Agree, 3 Disagree, 4 Abstain)As an aside, what's with the abstentions? the Chair and vice-chair and another member (Dr. Meadows) were ex officio members of the committee (probably due to their being state employees) but the report states that on the ASC subject they did vote. The report makes no mention of how each member voted or why those that abstained did so (I have this information but cannot confirm it). Given the high stakes involved I believe that some weaseled out of making a commitment. A few other reccommendations of note that do not relate to surgery, but may have a higher impact:
Abolish the exemption for physician-owned, office-based, single specialty ambulatory surgery centers and require such facilities to obtain a Certificate of Need under the exact same standards as all other ambulatory surgery centers.
The original recommendation of the Specialized Services Sub-Committee was to abolish the current ASC exemption and require all ASCs to obtain a Certificate of Need without exception. The full Commission discussed this recommendation, but was sharply divided and no final conclusion was reached on the recommendation.
and....
Recommendation 6.0 (4 Agree, 1 Disagrees, 5 Abstain)
Deregulate diagnostic cardiac catheterization and require therapeutic catheterizations to be performed only by providers approved to offer open heart surgery.
The members of the Commission who support the deregulation of adult diagnostic cardiac catheterization maintain that deregulating diagnostic cardiac catheterization will allow for the proliferation of these services in the market assuring access to residents in all areas of the state. Such members feel that this service is a valuable service to the citizens of the state and has been shown to save lives, particularly in states such as Georgia with high rates of coronary disease. These members feel that the regulation of the quality of this service could be managed by Licensure.
One member of the Commission disagrees. This member feels that this service should continue to be regulated by Certificate of Need. Because cardiac catheterization is such a specialized service, certain quality standards must be met to achieve the best possible outcomes. Because the American College of Cardiology recommends that minimum volumes be maintained to ensure the quality of the service, this member feels the Certificate of Need process ensures that there will not be a proliferation of low volume providers who won’t maintain the same quality as high volume providers.
Several members of the Commission report that this recommendation should only apply to hospital-based cardiac catheterization and not to freestanding cath programs.
Recommendation 7.0 (6 Agree, 1 Disagrees, 3 Abstain)The hospitals are already planning their next move:
Deregulate Level I perinatal services and continue regulation of Level II and Neonatal Intensive Care.
Most members of the Commission recommend that Level I perinatal services be deregulated because these services are already provided by most hospitals in the state and do not require specialized labor. These members believe that access to perinatal and obstetrical care will be enhanced by their recommendation. The fact that federal law already requires a facility to treat a woman in active labor further supports this recommendation. The members who make this recommendation maintain that Level II and Level III services should continue to be regulated by CON because of the highly- skilled nature of these services and the workforce that is required to support them. One member of this group further believed that Level II should be deregulated in addition to Level I.
One member of the Commission made the recommendation to maintain existing CON regulation for this service. This member believes that maintaining Certificate of Need regulation of Level I perinatal services will address the problem of large fixed costs incurred by facilities that provide these services and the shortage of skilled workforce.
Several members of the Commission report that this recommendation should be limited to Level 1 perinatal services at hospitals and should not be construed as a recommendation regarding freestanding facilities.
Concerned about a possible hit to their bottom line, metro Atlanta hospitals are preparing to put a few newly proposed state health-care regulations under the knife.
.....Hospitals argue that physician-owned surgery centers siphon off their best-paying patients, leaving the burden of the uninsured for hospitals to bear.
Recent financial data just released by the state Department of Community Health, which tracks the performance of hospitals each year, shows that metro Atlanta's 25 largest hospitals spent nearly $485 million combined on uncompensated, indigent and charity care in 2005. That's up 12 percent from $435 million in 2004.
The recommendation "is just one more knife in the hospitals' back, and it's a big knife," said Michael Rovinsky, president of the health-care consulting firm Integrity Consulting Group. "General surgery accounts for a lot of profitable procedures. This is the one [recommendation] that's going to be fought the hardest."
....But the proposal to classify general surgery as a single specialty could be damaging to many hospitals, especially as they continue to fight rising costs to care for the poor and uninsured.
"It would have a financial impact," said Holly Snow, Piedmont's vice president of government and external affairs.
The commission anticipated the controversy, and in its recommendations says all outpatient surgery centers must commit to serving the indigent and uninsured.
Other possibly contentious recommendations are also included in the commission report. One permits hospitals wanting to launch general labor and delivery programs to circumvent the certificate-of-need process. The same goes for hospitals trying to start up diagnostic heart catheterization programs. The catheterization procedure involves a thin, hollow tube that is threaded through the body to examine the heart's chambers.
My physician colleagues need to tread carefully here. The hospitals can make a very persuasive argument aimed at the public concerning lack of access to care. If left to their own devices I doubt many of these ASC's will take care of the medically complex or the underinsured. It will be an interesting battle.
Labels: Georgia
|Saturday, January 06, 2007
Innovative or Idiotic...
Is Dr. Parker ahead of the curve or delusional? Given the results of the match I participated in I myself have questions. Looking at the results from the latest surgery critical care match:
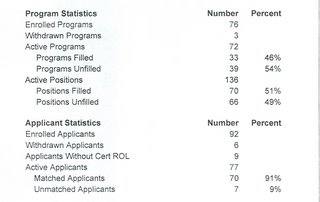
72 programs participated, out of 85 ACGME approved programs. Of these only 33 filled. On the other end 77 submitted rank lists for 136 postions, leaving a match rate of 91 percent and a fill rate of 51 percent. Now the picture painted here may not be too accurate because of the number of programs that did not partcipate in the match. There number of participants in the match may be underestimating the total number of fellows by as much as fifty percent given the numbers of those that have taken the certifying exam.
Anesthesia offers 54 ACGME approved fellowships in critical care. They do not participate in the match and I cannot find data from the certification examinations on the American Board of Anesthesia's website.
Let's take a look at the in internal medicine side. There are 29 critical care only programs that are certified by the ACGME, and 132 pulmonary medicine/critical care fellowships. Here is the NRMP data on the latest PM/CC match:
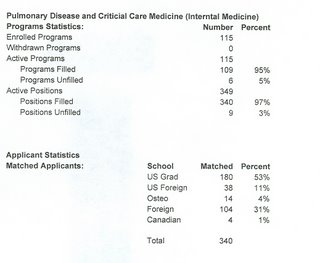
95 percent of programs filled and 97 percent of positions (340 out of 349) filled. This corresponds closely with the numbers who sit for the certifying exam. So the medical critical care track does seem to be more popular. The AAST is working on an acute care surgery curriculum, which is kind of what my practice plans of the future are. |
Is Dr. Parker ahead of the curve or delusional? Given the results of the match I participated in I myself have questions. Looking at the results from the latest surgery critical care match:
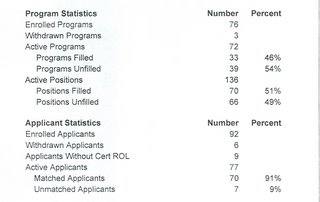
72 programs participated, out of 85 ACGME approved programs. Of these only 33 filled. On the other end 77 submitted rank lists for 136 postions, leaving a match rate of 91 percent and a fill rate of 51 percent. Now the picture painted here may not be too accurate because of the number of programs that did not partcipate in the match. There number of participants in the match may be underestimating the total number of fellows by as much as fifty percent given the numbers of those that have taken the certifying exam.
Anesthesia offers 54 ACGME approved fellowships in critical care. They do not participate in the match and I cannot find data from the certification examinations on the American Board of Anesthesia's website.
Let's take a look at the in internal medicine side. There are 29 critical care only programs that are certified by the ACGME, and 132 pulmonary medicine/critical care fellowships. Here is the NRMP data on the latest PM/CC match:
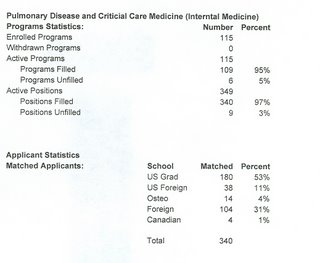
95 percent of programs filled and 97 percent of positions (340 out of 349) filled. This corresponds closely with the numbers who sit for the certifying exam. So the medical critical care track does seem to be more popular. The AAST is working on an acute care surgery curriculum, which is kind of what my practice plans of the future are. |
