Monday, October 30, 2006
Wednesday, October 25, 2006
From this month's Annals of Surgery the march of the specialty of "acute care surgery" moves on. An Acute Care Surgery Model Improves Outcomes in Patients With Appendicitis:
Objective: To compare outcomes of appendectomy in an Acute Care Surgery (ACS) model to that of a traditional home-call attending surgeon model.
Summary Background Data: Acute care surgery (ACS, a combination of trauma surgery, emergency surgery, and surgical critical care) has been proposed as a practice model for the future of general surgery. To date, there are few data regarding outcomes of surgical emergencies in the ACS model.
Methods: Between September 1999 and August 2002, surgical emergencies were staffed at the faculty level by either an in-house trauma/emergency surgeon (ACS model) or a non-trauma general surgeon taking home call (traditional [TRAD] model). Coverage alternated monthly. Other aspects of hospital care, including resident complement, remained unchanged. We retrospectively reviewed key time intervals (emergency department [ED] presentation to surgical consultation; surgical consultation to operation [OR]; and ED presentation to OR) and outcomes (rupture rate, negative appendectomy rate, complication rate, and hospital length of stay [LOS]) for patients treated in the ACS and TRAD models. Questions of interest were examined using χ2 tests for discrete variables and independent sample t test for comparison of means.
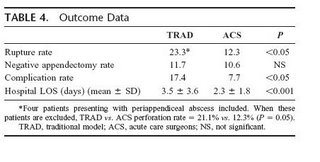
Results: During the study period, 294 appendectomies were performed. In-house ACS surgeons performed 167 procedures, and the home-call TRAD surgeons performed 127 procedures. No difference was found in the time from ED presentation to surgical consultation; however, the time interval from consultation to OR was significantly decreased in the ACS model (TRAD 7.6 hours vs. ACS 3.5 hours, P < 0.05); negative appendectomy rates were similar. The complication rate in the ACS model was decreased (TRAD 17.4% vs. ACS 7.7%, P < 0.05), as was the hospital LOS (TRAD 3.5 days vs. ACS 2.3 days, P < 0.001). Conclusions: In patients with acute appendicitis, the presence of an in-house acute care surgeon significantly decreased the time to operation, rupture rate, complication rate, and hospital length of stay. The ACS model appears to improve outcomes of acute appendicitis compared with a TRAD home-call model. This study supports the efficacy and efficiency of the ACS model in the management of surgical emergencies.
So having the in-house attending decreased ER time (elimnate those boarders), decreased rupures and complications, and decreases length of stay. All good things, no?
The "why" of acute care surgery is explained:
The future of trauma surgery as a career has become a topic of much debate in academic circles. Many factors have likely contributed to the relative shortage of trauma critical care surgeons. One recurring theme noted by a number of authors is the decreasing operative exposure for surgeons caring for injured patients. The predominance of nonsurgical management in blunt trauma and the decreasing incidence of penetrating trauma have resulted in a decreased operative experience in recent years. At the same time, emergency care is at a crisis, with widespread problems of access, overcrowding, boarding, and delays. Marked increases in emergency department visits by older, sicker patients, many with surgical emergencies, are more common and require a continuous workforce of surgical specialists to respond, evaluate, operate, and deliver critical care. Unfortunately, emergency departments are having significant and greater difficulties assuring specialist coverage. One recent report documents that over two thirds of emergency department directors report shortages of on-call specialists at their hospitals.
In response to these issues, many hospitals have had their trauma programs absorb emergency surgery into their practice.3,7 This model of acute care surgery (ACS), a combination of trauma surgery, broad-based emergency surgery, and surgical critical care, has been championed by the American Association for the Surgery of Trauma and a number of other trauma and surgical societies.2 A formal training curriculum is being developed, and plans for potential board certification are being explored. Several programs have reported their experience with the integration of emergency general surgery into their trauma programs. Most of these reports focus on surgeon satisfaction, surgeon caseload and diversity, and surgeon productivity. None, to date, has examined the effect of this integrated model on outcomes for patients with nontrauma surgical emergencies.
Here is a table of the timing data:
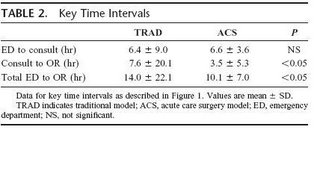
So the ACS group cut the consult to OR time by half, and the ED to OR time by almost a third. Here are some more figures with their accompanying text:
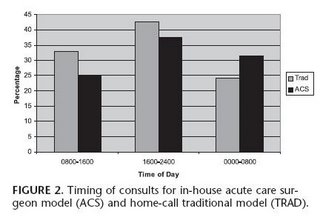

Surgical consultation occurred most frequently between 1600 and 2400 in both groups (Fig. 2). More than 30% of consultations in the ACS group occurred between 0000 and 0800. In contrast, more than 30% of consultations in the TRAD group occurred between 0800 and 1600. The timing of operative intervention is presented in Figure 3. More than 40% of surgeries in the TRAD group occurred between 1600 and 2400. In contrast, more than 40% of surgeries in the ACS group occurred between 0000 and 0800, compared with only 25% of surgeries in the TRAD group (P = 0.08). Of note, laparoscopic appendectomy was performed in only 10% of the ACS group and 6.5% of the TRAD group (P = not significant). One patient in each group required conversion to an open procedure
The results summarized:
Here is the discussion, emphasis is mine:
Caring for patients with surgical emergencies is one of the cornerstones of our profession. The potential to promptly diagnose an acute surgical problem and intervene in a timely fashion presents the surgeon with a unique opportunity to immediately impact a critically ill patient. As the population ages, the patients with surgical emergencies tend to have considerably more comorbid conditions and active medical problems. Unfortunately, these patients present at all hours of the day and night. They are challenging, time-consuming, and disruptive to the busy practicing surgeon. As a result, the surgeon's well-orchestrated and extremely efficient schedule of the day (outpatient office hours, elective surgical caseload, and for some, protected academic time) is often greatly disrupted by an emergent consultation. When emergent surgery is necessary, identifying available time in a busy OR schedule that does not further impact the surgeon's other responsibilities may be an additional challenge. Compounding this, many emergencies seem to occur on off hours and weekends, disrupting rest, family, and personal times. The possibility of being up all night or all weekend has both explicit and implicit effects on surgeons scheduling full clinical loads the following day. Finally, very little recognition or value can be currently found in academic surgical departments for taking on this difficult and complex patient population. Traditionally, the surgical trainee has played a major role in patient care during off hours. While the educational experience offered by this period of relative nonsupervision may be significant, the care rendered to those patients with surgical emergencies (arguably the ones who can least afford suboptimal or minimally supervised care) may be less than ideal. In many instances, faculty are only in phone contact with surgical trainees regarding emergent care of an acutely ill patient. Even at the academic medical center, the sickest emergency patient may not see a faculty surgeon for many hours during the crucial initial phases of emergency surgical care.
The acute care surgeon may be an answer to many of these and other issues prevalent in the current surgical setting. The backbone of such a program, the trauma and critical care surgeon, is already present at many medical centers. Seventy percent of level I trauma centers currently have 24/7 in-house faculty trauma surgeons.1 Because of the broad nature of injury, this specialty is already trained and familiar with a wide scope of surgical problems. In addition, more than 75% are trained and practice critical care so they have an expertise in the management of the comorbid conditions so often present in the emergent surgical patient. Expanding the trauma surgeon's role to a broader surgical emergency one has already begun to occur at a number of hospitals where emergency general surgery has been added to the responsibilities of the trauma surgeon. This new acute care surgeon can be at the bedside of the patient with a surgical emergency at a moment's notice. The experience that they bring to the bedside at all hours of the day and night should be beneficial to both the care of the ill surgical patient as well as the education of the surgical trainee.
Since this paper was presented at a meeting, the audience was able to ask questions. This one sums up, IMHO, the matter best:
Dr. Mark A. Malangoni (Cleveland, Ohio): Dr. Schwab, I certainly enjoyed your presentation and enjoyed reading the paper as well. This morning President Pellegrini alluded to the evolution of acute care surgery as a new surgical subspecialty, and you have presented high quality data that this model works in the care of a common surgical disease, acute appendicitis. The 4-hour reduction in time from the consultation to the operating room translates to a 47% risk reduction in rupture and a 56% risk reduction in complications as well as a one-day-shorter hospital stay, improvements that are hard to argue with.
If I was an acute care surgeon contemplating the importance of this new subspecialty, I would say these data unquestionably support the development of this new discipline. As a general surgeon, I would look at the data differently and I would conclude that it confirms that the existing information that reducing the delay from the time of diagnosis to the operating room in adults results in better outcomes, a fact that has been certainly supported by many previous studies as well as your current study. This strongly suggests that it is quality patient care, not surgeon convenience, that must take precedence.
I have a couple of questions for you. You have already addressed the issue of patient presentation at the emergency department and its potential impact. My 2 questions are: The acute care surgeons seem to get a greater number of consults between midnight and 8:00 am. Do you think the fact that the emergency medicine physicians knew that there was an in-house attending surgeon that would respond to consultation resulted in a propensity for them to call you and hence may have decreased the time to consultation for the acute care surgeon and may have affected the results?
Second, we all know that this acute care surgery model is still controversial, particularly in nonteaching hospitals, where there are fewer surgical subspecialists. Now, if you believe that all hospitals should have acute care surgeons, could you expand a bit upon how that would occur? If you feel that this is a model that only should apply to those of us who work in teaching hospitals where there may be a greater number of surgical subspecialists, what should be done in the community hospitals where there is less likely to be a trained acute care surgeon present?
The highlighted quote reminds me of a summary post of another paper that the greatest advantage of the acute care surgeon was seen by the "somnolent elective surgeon". The reply:
Dr. C. William Schwab (Philadelphia, Pennsylvania): First of all, I don't know if the Yogi Berra element was in work here. And that is, you know, showing up is 89% of the game. I just don't know if that was true.
I will tell you that the way the emergency physicians consulted the surgical service did not change whether it was a month in which the acute care surgery model was in place or the traditional model was in place. The consults came to a third-year surgical resident, he responded, sought consultation if necessary from a more senior surgical resident and at that point we were brought in, meaning the faculty. The fact that we were there, I just can't say. And as I said but didn't explain it, I wish this was a time-in-motion study in which I could provide you all hour to hour what was going on in the management of these cases. I can't. And this is really looking at that from really, I think, 37,000 feet.
The next question you asked is, do I think this is a model that works only in a teaching hospital? For me to speculate on that is looking into a crystal ball. I will tell you that I have 2 colleagues that are in trauma critical care, both of whom have been recruited from academic surgery into the community practice and specifically hired by hospitals with the consent, approval and support of the departments of surgeries in these community hospitals to establish an acute care surgical model to relieve them of all the burden of the ED and the trauma patients.
It is an interesting observation. I personally do not think that this model is only for the academic medical centers or teaching hospitals. I think it is applicable to any particular hospital. I also don't think it is applicable only for surgeons that have special training in critical care and experience in trauma. I think any general surgeon broadly based and well trained with an interest can be an acute care surgeon. I think we ought to design to train the future generations with the curriculum that the AAST is developing, but we need to stay tuned for what that looks like.
The acute care surgeon concept benefits the hospital by having a group of dedicated surgeons who will respond to the emergency room. It benefits the interested surgeon because it allows for regularity of schedule. With specialist coverage of ED's becoming an increasing problem, and the regulated schedules of current trainees I believe that over time this model will become more widespread and accepted. I know that my colleague in the Rocky Mountains may disagree.
Now in my last post on this subject I did not mean to imply that those who enjoyed surgery, but did not pursue a residency were lazy, but that in my experience those who left my training program were discontents which were best described as "lazy". I think that even if "surgical hospitalists" become more prevalent, that "part-time" training won't catch on. This is a solution in search of a problem now, but maybe not a few years ago. Look at how surgery has fared in the match over the past few years: (click to enlarge)

What changed between 2002 and 2003? Workhour limits. So the "lifestyle sensitive" have started to join up.
Labels: appendicitis, Future of Surgery
|Tuesday, October 24, 2006
Monday, October 23, 2006
With a hat-tip to Kevin here are my two cents worth on what he calls the "softening" of surgical residency. The article from Forbes:'Flex' Training Can Boost Number of Surgeons:
Medical students studying surgery often quit before completing their training. Now, a new study suggests that schools that offer part-time and other flexible training options could boost and maintain students' interest in surgery.But are these the surgeons you want to care for you or your family members?
The Web-based survey also found that some residents, fellows and practicing surgeons also would be interested in flexible training options.
"Many of today's medical students have more diverse interests and, when they apply for postgraduate training, may prefer specialties in which a more flexible approach to training (i.e., part time, reduced hours or extended period of time off) is an option to allow them to integrate other professional and family interests," wrote a team from the University of Virginia Health System in Charlottesville.
Currently in the United States, surgical residencies last a minimum of five years. As many as 20 percent of surgical residents quit their programs before they finish. In most cases, lifestyle concerns are the reason, according to background information in article.And in other cases they fail to measure up academically or find they are unsuited for surgery as a career. "Lifestyle concerns" strikes me as a catch-all term for those who are too lazy or don't have the personality to survive through a surgical residency. If my personal experience is a guide, the eighty percent who graduate don't miss the twenty-percent who didn't very much.
Of the 4,308 medical students and doctors who took part in the survey, 20 percent to 30 percent said they'd accept a residency that lasted longer than five years if they could train part time, but few said they'd accept an extension to more than seven years.What would they do when they weren't surgical residents? The reason that residency is at least five years is because it takes that long to acquire the operative experience to become proficient at a procedure. Performing one, two, or even ten appendectomies does not make one an expert. There is a great possibility that without constant exposure during the "formative years" of one's residency that skills will not be as developed as they should be. Now for the "money graf":
The survey also found that 36 percent of female and 24 percent of male medical students said a more flexible approach to training would make them more likely to choose a career in surgery.
"In light of recent concerns about decreasing applications to general surgery training programs and a need to appeal to students with greater interest in controllable lifestyle careers, a more flexible approach to surgical training could boost interest and improve applicant caliber," the authors noted.(Emphasis mine)
So in order to appeal to the minority who would really like to become surgeons except for the sacrifice and time commitment required, we will make it a part-time experience. As some commenters to Kevin's post point out, general surgery remains very competitive. As seen in the 2006 match, only one slot went unfilled nationwide. Here are some figures from the 2005 match:
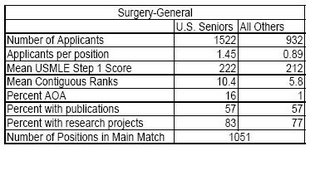
So are does this paper offer a solution for a problem that does not exist? Maybe maybe not. With close to eighty percent of chief residents pursuing fellowship training of one form or another maybe extending the training would encourage more residents to stick with general surgery. I doubt it though, while the residency my be part-time one would be hard-pressed to find a part time private practice job right now. Maybe not so hard in the future. The patient population wants knowledgeable, well-rested, and attentive physicians. With the 80-hour workweek limits in training and the habits learned under that system spreading to the "real world", two out of three isn't bad.
The abstract to the Archives of Surgery paper is here.
Labels: Future of Surgery
|Sunday, October 22, 2006

Georgia 27 Mississippi State 24
As the article points out, we are bowl eligible. But next week in Jacksonville won't be pretty sa it stands.
Labels: Bulldogs, college football
|Thursday, October 19, 2006
We already know that obesity can be a hindrance in diagnosis. And in this month's Journal of the American College of Surgeons are two papers which discuss how obesity affects outcomes after trauma. The first: Impact of Obesity in the Critically Ill Trauma Patient: A Prospective Study
Background
Obesity has risen at an epidemic rate over the past 20 years in the US. To our knowledge, there is an absence of data evaluating the impact of obesity in the critically ill trauma patient.
Methods
Prospective data were collected on 1,167 patients admitted to the ICU over a 2-year period. Obesity was defined as a body mass index (calculated as weight [kg]/height [m2]) of 30 or higher. Outcomes analyzed included infection rate, hospital and ICU length of stay, and mortality. Multiple logistic regression was used to evaluate outcomes between obese and nonobese patients for infection (infection versus noninfection) and mortality (deceased versus not deceased). Continuous outcomes such as hospital and ICU lengths of stay were evaluated using multiple linear regression analyses.
Results
Sixty-two of 1,167 (5.3%) patients were obese. The majority (71%) of injuries in the study cohort were blunt. Although the majority of patients were men (76%), women (10% versus 4%) were more likely to be obese (p < 0.001). Obese patients had a more than twofold increase in risk of acquiring a bloodstream, urinary tract, or respiratory infection, or being admitted to the ICU (p < 0.001), after statistically controlling for age and Injury Severity Score. When controlling for diabetes, gender, obesity, age, COPD, and Injury Severity Score, obese patients were 7.1 times (95% CI, 2.06Â8.9) more likely to die in the hospital.
Conclusions
Obesity is associated with a substantial increase in morbidity and mortality in the critically ill trauma patient. Future studies are warranted in both the prevention of infection and intensive care management of the obese trauma patient.
Unfortunately the JACS does not place their tables on the HTML version as pictures, so I am unable to grab any graphics from the article. Due to my inferior skills I am also unable to cut and paste the information and get the margins lined up correctly. My apologies. The data show that obesity is as strong a risk factor as age, diabetes, or COPD concerning total LOS as well as ICU LOS.
From the discussion:
The nature of substantial body mass has an impact on how health care providers deliver their care. In our study, we have shown that obese patients have a considerably greater number of ventilator days and pneumonia. This might be, in part, because of an intrinsic reduced lung capacity and increased work of breathing. These patients are also at greater risk of aspiration pneumonia. Procedures such as endotracheal intubation or tracheostomy are quite challenging because of immobility or thickness of subcutaneous tissue of the neck. These factors can play a role in delaying tracheostomy, potentially increasing ventilator days.
Vascular access in obese patients can also present a challenge to the health care provider. Difficulty in maintaining peripheral IV sites increases use of central venous catheters. Placement of central lines can be difficult because of lack of physical landmarks and increased distance to vessels. In critically ill obese patients, the persistent need for venous access is common and promotes the practice of longterm central access. This practice can increase the risk of line sepsis, as demonstrated in our study.
Obese patients have been shown in our study, as monitoring urine output continues to be an important part of ICU care, to have a considerably greater number of Foley catheter days. This almost certainly accounts for the more than twofold risk in urinary tract infections in our obese patients.
As we turn the page we find this article:Obesity Increases Risk of Organ Failure after Severe Trauma:
Background
Obesity is an independent risk factor for a variety of diseases, including postinjury morbidity and mortality. Obesity is associated with a proinflammatory state that could affect the postinjury inflammatory response and increase risk of organ dysfunction. The purpose of this study was to determine the relationship between obesity and postinjury multiple organ failure (MOF).
Study design
A prospective observational study of patients at risk for postinjury MOF. Inclusion criteria were age older than 15 years, Injury Severity Score > 15, ICU admission within 24 hours of injury, and survival longer than 48 hours after injury. Isolated head injuries were excluded. Organ dysfunction was assessed using the Denver multiple organ failure score.
Results
Data were collected on 716 severely injured patients, 70% were men and 83% were victims of blunt trauma. There was no relationship between body mass index and injury severity or the amount of blood transfused within 12 hours of injury. Postinjury MOF was observed in 123 of 564 (22%) nonobese patients and 56 of 152 (37%) obese patients. Obesity was independently associated with MOF (odds ratio, 1.8; 95% CI, 1.2–2.7) after adjusting for patient age, injury severity, and amount of blood transfused during resuscitation. In this study population, obesity was also associated with increased length of ICU and hospital stay but not death.
Conclusions
Obese patients are at increased risk of postinjury MOF. Study of the obesity-related inflammatory profile could provide additional insight into the pathogenesis of organ dysfunction and identify therapeutic targets for both obese and nonobese patients. Increased morbidity and length of stay in obese trauma patients implies greater resource allocation for this population.
Again, the spacing on the tables doesn't translate well to cut-and-paste, but the authors give some indication as to why this occurs:
When multiple systems were evaluated, we found that postinjury MOF was 1.8 times more likely to develop in obese patients than nonobese patients after adjusting for the previously established risk factors. Obesity was found to confer an increased risk of postinjury MOF greater than that of severe injury. MOF was more likely to develop within 72 hours of injury in obese patients than nonobese patients. Because early MOF is thought to reflect the effects of unbridled postinjury hyperinflammation as opposed to uncontrolled infection, this observation supports the proinflammatory nature of the obese state. Alternatively, early organ dysfunction could represent decreased physiologic reserve of these patients. Of those in whom MOF developed, there were no differences in the spectrum of involved organs between obese and nonobese patients. The lung was the most frequent organ involved, followed by the heart, liver, and kidney. It is interesting that once the threshold for MOF is reached, obese patients display the same organ dysfunction pattern as nonobese patients. This might be evidence that the final common pathway to postinjury organ dysfunction is not different between obese and nonobese patients. We conclude from these observations and previous research that obesity is associated with a proinflammatory state that influences the postinjury inflammatory response and resultant organ dysfunction.
And finally:
In summary, we found that obesity is a strong independent risk factor for postinjury organ dysfunction and MOF. These findings, in conjunction with evidence for an altered inflammatory potential in obese patients, might point to therapeutic targets to improve outcomes in both obese and nonobese patients. Finally, the shift toward a more obese population could affect use of trauma and critical care resources because of the higher risk of postinjury MOF.|
Wednesday, October 18, 2006
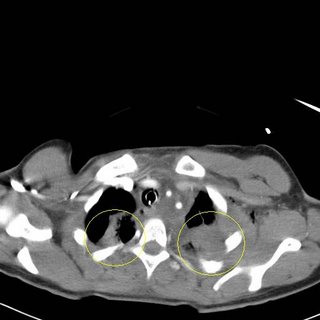
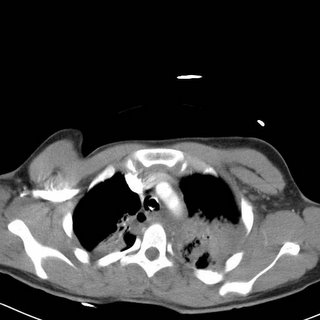
Patient in a motor-vehicle collision. Rollover with ejection. Flown in and intubated shortly after arrival.


Something is here that doesn't belong. From the plates inidcated by the yellow lines
we can see that this patient has been a guest of the trauma service before. More images to follow:




Brain windows on the head CT. Whatever it is it appears to pass over the globe and enter the frontal lobe with associated hemorrahge. Here is the bone window of the third image:

You can make out the fracture of the orbital roof. Here are the recontstructions from the facial CT:


Here's the best of these:

And now for the really cool images:


These are from the 3-D recons. The blue line indicates the offender. Here is the obligitory live action shot:
WARNING !!! THE FOLLOWING MAY BE OFFENSIVE:

The object in question is just above the eyelid. The patient was taken off to the OR by the neurosurgeons for removal and placement of an ICP monitor. What was it? Probably the swivel mount from a rear-view mirror.
Labels: Tales from the Trauma Service
|Tuesday, October 17, 2006
Monday, October 16, 2006
Catching up on my reading I found this in the June issue of The Journal of Trauma:Helicopter Scene Transport of Trauma Patients with Nonlife-Threatening Injuries: A Meta-Analysis:
Background: Helicopters have become a major part of the modern trauma care system and are frequently used to transport patients from the scene of their injury to a trauma center. While early studies reported decreased mortality for trauma patients transported by helicopters when compared with those transported by ground ambulances, more recent research has questioned the benefit of helicopter transport of trauma patients. The purpose of this study was to determine the percentage of patients transported by helicopter who have nonlife-threatening injuries.
Methods: A meta-analysis was performed on peer-review research on helicopter utilization. The inclusion criteria were all studies that evaluated trauma patients transported by helicopter from the scene of their injury to a trauma center with baseline parameters defined by Injury Severity Score (ISS), Trauma Score (TS), Revised Trauma Score (RTS), and the likelihood of survival as determined via Trauma Score-Injury Severity Score (TRISS) methodology.
Results: There were 22 studies comprising 37,350 patients that met the inclusion criteria. According to the ISS, 60.0% [99% confidence interval (CI): 54.5-64.8] of patients had minor injuries, According to the TS, 61.4% (99% CI: 60.8-62.0) of patients had minor injuries. According to TRISS methodology, 69.3% (99% CI: 58.5-80.2) of patients had a greater than 90% chance of survival and thus nonlife-threatening injuries. There were 25.8% (99% CI: -1.0-52.6) of patients discharged within 24 hours after arrival at the trauma center.
Conclusions: The majority of trauma patients transported from the scene by helicopter have nonlife-threatening injuries. Efforts to more accurately identify those patients who would benefit most from helicopter transport from the accident scene to the trauma center are needed to reduce helicopter overutilization.
What they did was analyze the above studies to determine if, based on objective criteria, patients would benefit from a helicopter transport. For those not familiar with the criteria here is an explanation:
The ISS is an anatomic scoring system for patients with multiple injuries and does not include physiologic variables. The ISS ranges from 0 to 75 with the severity of injury and mortality increasing with the score. Patients with an ISS >15 are deemed to require specialized trauma care while patients with an ISS of 15 or less are considered to have nonlife-threatening injuries. The original TS included four physiologic parameters (respiratory rate, respiratory expansion, systolic blood pressure, capillary refill) and the Glasgow Coma Scale (GCS). It had a range from 1 to 16 points. Patients with a score of 12 or less were deemed to be seriously injured and required specialized trauma care. The TS was revised in 1989 and became the RTS. Two of the physiologic parameters (respiratory expansion and capillary refill) were dropped. The range of the RTS is 0 to 12. Patients with a score of 11 or less are deemed to require specialized trauma care. While the RTS is most commonly used in the prehospital setting, a weighted form of the scale is used to predict patient outcomes following trauma. With the weighted RTS, greater emphasis is placed on the GCS. The range for the weighted RTS is 0 to 7.8408. Higher scores are associated with a better prognosis. Patients with a weighted RTS score of <4 are felt to benefit from specialized trauma care while patients with a score of ≥4 are generally considered to have minor injuries. The TRISS system combines the RTS, the ISS, the patient's age, and the type of trauma sustained (blunt or penetrating) to determine a probability of survival (P s)
Not all of those scoring systems were used in all of the studies so the ISS, TS, and TRISS were evaluated. The severity criteria were as follows:
To determine which patients were unlikely to benefit from helicopter transport, we used the standard trauma scoring systems described above. Based upon validated criteria, patients having a TS ≥13, a RTS >11, a weighted RTS ≥4, and/or an ISS ≤15 were deemed to have sustained nonlife-threatening injuries and therefore did not require helicopter transport. Likewise, a TRISS-derived probability of survival (P s) of greater than 0.90 (a 90% or better chance of survival) also represents nonlife-threatening injuries and was included as one of the inclusion criteria. Finally, patients who were discharged from the emergency department or hospital within 24 hours of admission for trauma are generally considered to have nonlife-threatening injuries and were included in the inclusion selection criteria.
So, looking at the first set of data:
As you see the range of patients with an ISS at or below 15 ranges from 85.1 percent to 34.6 percent, with a mean of 60 percent. So by this reckoning, sixty percent of these patients did not have an injury severity high enough to justify helicopter transport. Moving along:
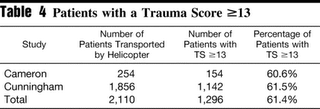
Three studies used the trauma score as the criteria. All had over sixty percent of their patients with a trauma score greater than 13. So, by their criteria, only fort percent of the patients required helicopter transport. This appears consistent with the results above.
Here the TRISS is examined. A patient with a P> 90 has a greater than 90 percent chance of survival, and should not require helicopter transport. The percentage ranges from 41.9 to 90 percent with an average of 69.3 percent. So by this criteria almost 7 out of 10 patients should not have required helicopter transport.
This is the "what, no helicopter ride home?" group. The percentages here are not as large, perhaps due to the "non-standard" criteria.
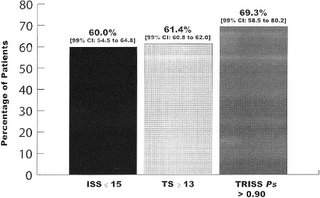
Here is a comparison of the "minor injuries" based on scoring system. They seem to compare well.
So why are all of these patient's riding the whirlybird? The authors opine:
Our study demonstrated that the majority of trauma patients transported by medical helicopter from the scene had nonlife-threatening injuries. We believe there are two possible explanations for this phenomenon. First, there may be a significant degree of overutilization of helicopter scene flights for trauma by air-medical services despite quality assurance oversight that reveals these flights to be nonbeneficial. Second, and more probable, the apparent overutilization may be because of a significant degree of overtriage in the field by prehospital providers resulting in inappropriate requests for helicopter scene transport.
There are concerns about helicopter safety:
There has been a marked increase in the number of medical helicopter accidents in the United States. In fact, half of all accidents in one 10-year study (1993-2002) occurred during the last 3 years of the study period. Because of the lack of a centralized database, it is impossible to determine whether this increase in accidents reflects a decline in operational safety or merely reflects the fact that there are more aircraft flying more missions. In January of 2005, in response to a sharp increase in fatal medical helicopter accidents, the NTSB and the Federal Aviation Administration (FAA) launched safety reviews of medical helicopters.
The authors provide an explanation for the change in the results of the studies:
It is curious that early studies demonstrated that helicopter transport decreased mortality from trauma while more recent studies have indicated little or no benefit from helicopter transport. The authors believe this reflects the tremendous improvements in ground prehospital care observed over the last 20 years including more widespread advanced life support units and markedly enhanced EMT and paramedic education. Other factors that may explain this difference include improved categorization of hospitals, the organization and implementation of regional trauma systems, trauma centers, and postgraduate educational programs that specialize in trauma care.The authors then list the limitations of the study, the last IMHO is the most relevant (emphasis mine)
Fourth, current helicopter utilization criteria are applied at the scene of trauma while the ISS is calculated retrospectively once the patient has received definitive care. The use of the ISS has been reported to not identify a subset of trauma patients who may benefit from definitive trauma care. However, the ISS is usually applied retrospectively following hospital admission and is not routinely used for prehospital trauma triage decision making. The ISS is the scoring system most commonly used in the studies referenced in this article.
The use of the TRISS system has both benefits and limitations. TRISS is widely used and validated. However, it is applied retrospectively and does not aid prehospital personnel in determining which patients may actually benefit from helicopter transport. Furthermore, the TRISS has been reported to overestimate survival in patients who are severely injured. However, in our cohort we were interested in patient with minor injuries.
So the old struggle of overtriage/undertriage strikes again. Field decisions are made based on physiologic status and mechanism of injury (MOI). MOI can overestimate severity, and can be overly sensitive. I myself believe that helicopter transport is overutilized and some restraint would be helpful from time to time.
See also:
Send the Whirlybird
Send the Whirlybird II |
Sunday, October 15, 2006
At around 11:30 last night ACTCIACTC had its' 200,000th visitor. I do think that counts the thousands of times each day my mom loads the page, however. Thanks for all who have paid a visit over the past three years. |

Georgia 22 Vanderbilt 24
Glad I didn't go to the game yesterday. Complete meltdown as the article indicates. If the Dogs continues as is, the Florida and Auburn games will be bloodbaths.
But I'm not as fed up as these guys are.
But at least it didn't sink to the level of this (click on video to watch).
UPDATE: Here it is with the obnoxious commentary by the (now forner) color commentator for CSS sports, Lamar Thomas.
|
Friday, October 13, 2006
Patient shot in the back at unknown range. Allegedly with a .223 caliber round. Here is the initial x-ray:
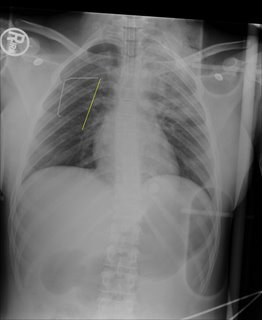
The yellow line (and paperclip) indicates the entry wound on the patient's back. Now as for the exit, that will be revealed shortly. Here are some additional images:
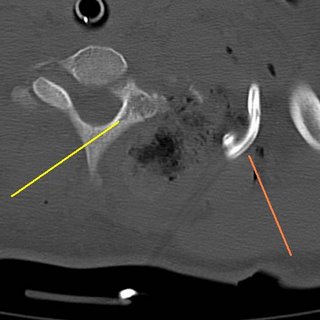
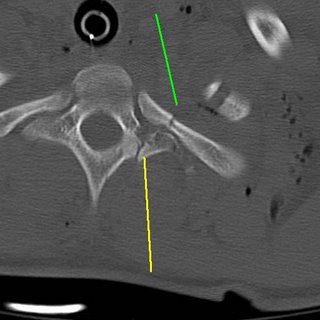
The yellow line represents a lamina fracture of the first thoracic verterbra. No hints on what the green line points to.
Transverse process fracture (yellow) and an associated rib fracture (green).
Bilateral pulmonary contusions, left greater than right. There is also some blood in the left hemithorax.
The contusions continue. Now for what you have been waiting for:
WARNING, POTENTIALLY OFFENSIVE IMAGES FOLLOW:
YOU HAVE BEEN WARNED!!!
Here is the exit on the anterior neck:
With a 6cc syringe for comparison:

The structure at the anterior of the wound is the posterior border of the sternocleidomastiod (SCM) muscle. I was able to digitally explore the wound and able to palpate inferior to the fractures seen in the CT scans above. Bleeding was primarily from fractured bone and torn muscle. No injury of the carotid, jugular vein, esophagus or trachea was seen. The wound was irrigated, packed with gelfoam and surgicel and I placed a Jackson-Pratt drain (that's what the green line was indicating).
But something very important does live there:
The brachial plexus. Here is some of the anatomy of the area:
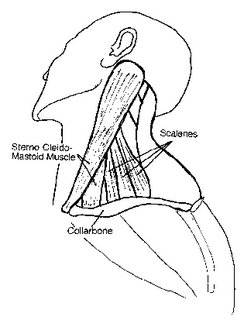
From this diagram we can see the scalene muscles which lie posterior to the SCM. Those were pretty much destroyed by the blast. This next diagram

The brachial plexus also lies here. The phrenic nerve (which controls the diaphragm) does too. Prior to intubation the patient had no motor or sensory function of their left arm. We will probably obtain an EMG next week.
Labels: Tales from the Trauma Service
|Thursday, October 12, 2006

Tennessee is Doomed.....
Look who made the cover of S.I. this week:

That's Georgia punter Gordon Ely-Kelso in the backgound, BTW. |
Gotta love Dr. Gawande. Dr. Pho yesterday linked to a New Yorker article about "how childbirth went industrial" :THE SCORE. What follows is a informative look a the history of obstetrics (which I highly encourage you to read) and how things as forceps delivery and the Apgar score have improved outcomes for both mothers and babies:
Around the world, virtually every child born in a hospital had an Apgar score recorded at one minute after birth and at five minutes after birth. It quickly became clear that a baby with a terrible Apgar score at one minute could often be resuscitated—with measures like oxygen and warming—to an excellent score at five minutes. Spinal and then epidural anesthesia were found to produce babies with better scores than general anesthesia. Neonatal intensive-care units sprang into existence. Prenatal ultrasound came into use to detect problems for deliveries in advance. Fetal heart monitors became standard. Over the years, hundreds of adjustments in care were made, resulting in what’s sometimes called “the obstetrics package.” And that package has produced dramatic results. In the United States today, a full-term baby dies in just one out of five hundred childbirths, and a mother dies in one in ten thousand. If the statistics of 1940 had persisted, fifteen thousand mothers would have died last year (instead of fewer than five hundred)—and a hundred and twenty thousand newborns (instead of one-sixth that number).So along with anesthesia they have improved their oucomes. But according to Dr. Gawande the approach does not exactly fit the conventional "evidence based" approach:
In obstetrics, meanwhile, if a strategy seemed worth trying doctors did not wait for research trials to tell them if it was all right. They just went ahead and tried it, then looked to see if results improved. Obstetrics went about improving the same way Toyota and General Electric did: on the fly, but always paying attention to the results and trying to better them. And it worked. Whether all the adjustments and innovations of the obstetrics package are necessary and beneficial may remain unclear—routine fetal heart monitoring is still controversial, for example. But the package as a whole has made child delivery demonstrably safer and safer, and it has done so despite the increasing age, obesity, and consequent health problems of pregnant mothers.But with the ease one can figure an Apgar score, and obtain a "whole picture" assesment of the baby's status, comparisons will be made. And that has a wide impact: (emphasis mine)
The Apgar effect wasn’t just a matter of giving clinicians a quick objective read of how they had done. The score also changed the choices they made about how to do better. When chiefs of obstetrics services began poring over the Apgar results of their doctors and midwives, they started to think like a bread-factory manager taking stock of how many loaves the bakers burned. They both want solutions that will lift the results of every employee, from the novice to the most experienced. That means sometimes choosing reliability over the possibility of occasional perfection.And some things are easier taught than others.
The main point, and main question, of the article IMHO lies here:The fate of the forceps is a revealing example. I spoke to Dr. Watson Bowes, Jr., an emeritus professor of obstetrics at the University of North Carolina and the author of a widely read textbook chapter on forceps technique. He started practicing in the nineteen-sixties, when fewer than five per cent of deliveries were by C-section and more than forty per cent were with forceps. Yes, he said, many studies did show fabulous results for forceps. But they only showed how well forceps deliveries could go in the hands of highly experienced obstetricians at large hospitals. Meanwhile, the profession was being held responsible for improving Apgar scores and mortality rates for new-borns everywhere—at hospitals small and large, with doctors of all levels of experience.
“Forceps deliveries are very difficult to teach—much more difficult than a C-section,” Bowes said. “With a C-section, you stand across from the learner. You can see exactly what the person is doing. You can say, ‘Not there. There.’ With the forceps, though, there is a feel that is very hard to teach.” Just putting the forceps on a baby’s head is tricky. You have to choose the right one for the shape of the mother’s pelvis and the size of the child’s head—and there are at least half a dozen types of forceps. You have to slide the blades symmetrically along the sides, travelling exactly in the space between the ears and the eyes and over the cheekbones. “For most residents, it took two or three years of training to get this consistently right,” he said. Then a doctor must apply forces of both traction and compression—pulling, his chapter explained, with an average of forty to seventy pounds of axial force and five pounds of fetal skull compression. “When you put tension on the forceps, you should have some sense that there is movement.” Too much force, and skin can tear, the skull can fracture, a fatal brain hemorrhage may result. “Some residents had a real feel for it,” Bowes said. “Others didn’t.”
The question facing obstetrics was this: Is medicine a craft or an industry? If medicine is a craft, then you focus on teaching obstetricians to acquire a set of artisanal skills—the Woods corkscrew maneuver for the baby with a shoulder stuck, the Lovset maneuver for the breech baby, the feel of a forceps for a baby whose head is too big. You do research to find new techniques. You accept that things will not always work out in everyone’s hands.This is what is meant by "industrial medicine". Protocol-driven, evidence-based plans for what ails you. Because of this the vast majority of patients will be treated the same way for the same condition wherever they are. Some friends of mine have a child with lymphoma and they asked me if they should get treatment from the pediatric oncologist here or go to a referral center. Because of what I have described above I reccommended they remain here. The treatment will be the same and they (and their child) can remain at home surrounded by familiarity and people to help them.
But if medicine is an industry, responsible for the safest possible delivery of millions of babies each year, then the focus shifts. You seek reliability. You begin to wonder whether forty-two thousand obstetricians in the U.S. could really master all these techniques. You notice the steady reports of terrible forceps injuries to babies and mothers, despite the training that clinicians have received. After Apgar, obstetricians decided that they needed a simpler, more predictable way to intervene when a laboring mother ran into trouble. They found it in the Cesarean section.
The diagnosis of appendicits used to require years of training and experience, to know how to examine a patient and pick up on the subtle cues to determine the diagnosis, along with a few bad outcomes to provide negative re-enforcement. Now with CT scanners the diagnosis is made quickly and often before the surgeon is involved. Are there still "superstars" out there? Yes, and has been pointed out here before with certain procedures, volume makes a big difference. But in the performance of common procedures the difference between "great" and "good enough" is small. Don't belive me? Ask this guy. With the technology that exists (plugs and patches) your workaday general surgeon can approach recurrence rates that rival the Shouldice Hospital, without the trip to Canada.
Back to the article:
Yet there’s also no getting around C-sections. We have reached the point that, when there’s any question of delivery risk, the Cesarean is what clinicians turn to—it’s simply the most reliable option. If a mother is carrying a baby more than ten pounds in size, if she’s had a C-section before, if the baby is lying sideways or in a breech position, if she has twins, if any number of potentially difficult situations for delivery arise, the standard of care requires that a midwife or an obstetrician at least offer a Cesarean section. Clinicians are increasingly reluctant to take a risk, however small, with natural childbirth.
I asked Dr. Bowes how he would have handled obstructed deliveries like Rourke’s back in the sixties. His first recourse, as you’d expect, would have included forceps. He had delivered more than a thousand babies with forceps, he said, with a rate of neonatal injury as good as or better than with Cesarean sections, and a far faster recovery for the mothers. Had Rourke been under his care, the odds are excellent that she could have delivered safely without surgery. But Bowes is a virtuoso of a difficult instrument. When the protocols of his profession changed, so did he. “As a professor, you have to be a role model. You don’t want to be the cowboy who goes in to do something that your residents are not going to be able to do,” he told me. “And there was always uncertainty.” Even he had to worry that, someday, his judgment and skill would fail him.
These were the rules of the factory floor. To discourage the inexpert from using forceps—along with all those eponymous maneuvers—obstetrics had to discourage everyone from using them. When Bowes finished his career, in 1999, he had a twenty-four-per-cent Cesarean rate, just like the rest of his colleagues. He has little doubt that he’d be approaching thirty per cent, like his colleagues today, if he were still practicing.
Will mediocraty be the norm? Only time will tell. |
Wednesday, October 11, 2006
A few weeks ago the media was abuzz about a paper mill worker from North Carolina who was being sent by his company to India for a rotator cuff repair and a cholecystectomy. He was excited as he had a few days of sightseeing planned before his surgery. There were also significant cost savings involved. From the Christian Science Monitor, Companies explore overseas healthcare
Carl Garrett, a paper-mill technician in Leicester, N.C., is scheduled to travel Sept. 2 to New Delhi, where he will undergo two operations. Though American individuals have gone abroad for cheaper operations, Mr. Garrett is a pioneer of sorts.
He is a test case for his company, Blue Ridge Paper Products, Inc., in North Carolina, which is set to provide a health benefit plan that allows its employees and their dependents to obtain medical care overseas beginning in 2007.
"It's brand-new and nobody's ever heard of going to India or even South Carolina for an operation, so it's all pretty foreign to people here," says Garrett. "It's a frontier."
Garrett's medical care alone may save the company $50,000. And instead of winding up $20,000 in debt to have the operations in the US, he may now get up to $10,000 back as a share of the savings. He'll also get to see the Taj Mahal as part of a two-day tour before the surgery.
His two operations could cost $100,000 in the US; they'll run about $20,000 in India.
First off, I have no idea what the professional or facility fees are for rotator cuff surgery, but rest assured this man could come to River City and have his gallbladder out for much less than $50K. The "outsourcing" of patients is becoming more popular.
Insurers Health Net of California already contracts with medical clinics on the Mexico side of the US border.Mr. Garret was excited about the trip. But as it turns out, the United Steelworkers of America threw a flag on the play. From today's New York Times, Union Disrupts Plan to Send Ailing Workers to India for Cheaper Medical Care:
A West Virginia state legislator introduced a bill this year that would encourage state workers to seek treatment overseas using incentives such as cash bonuses and family travel.
United Group Programs in Florida, which administers self-insurance programs for small companies, has contracted with a Thailand hospital for its employer clients.
Inquiries from self-insured employers are brisk at IndUShealth in Raleigh, N.C., which specializes in offshoring serious medical cases such as rotator cuff surgery and gall bladder removal to India.
A few weeks ago, Carl Garrett, a 60-year-old North Carolina resident, was packing his bags to fly to New Delhi and check into the plush Indraprastha Apollo Hospital to have his gall bladder removed and the painful muscles in his left shoulder repaired. Mr. Garrett was to be a test case, the first company-sponsored worker in the United States to receive medical treatment in low-cost India.The union's objection has to do with the liability question. Mr. Garrett had signed a waiver of liability for the company should anything go awry:
But instead of making the 20-hour flight, Mr. Garrett was grounded by a stormy debate between his employer, which saw the benefits of using the less expensive hospitals in India, and his union, which raised questions about the quality of overseas health care and the issue of medical liability should anything go wrong.
"I was looking forward to the adventure of being treated in India," Mr. Garrett said the other day. "But my company dropped the ball."
The union, the United Steelworkers, stepped in after it heard about Mr. Garrett's plans, saying it deplored a "shocking new approach" of sending workers to low-cost countries as a way to cut health care costs. Its officials insisted that Mr. Garrett be offered a health care option within the United States.
"No U.S. citizen should be exposed to the risks involved in traveling internationally for health care services," Leo W. Gerard, the president of the union, said in a recent letter to the Senate and House committees that oversee health care. He expressed his concern about the willingness of employers to offer incentives to employees to go overseas.
Still, cross-border medical liability in countries like India could prove to be a major hurdle, the experts say. In the case of Mr. Garrett, Blue Ridge Paper asked him to sign a release saying that he was "on his own as far as medical liability," said Bonnie Blackley, the benefits director at Blue Ridge.The union is just shocked, shocked that such a thing would even be considered:
But United Steelworkers, the largest industrial union in North America with over 850,000 members, said it would fight any effort by American companies to send employees abroad for treatments. "We are confident that we are in a position to block any employees being exported to India, Thailand or Mexico," said Stan Johnson, a spokesman. "The ailing American health care system cannot be cured by sending patients abroad."But as the CSM article points out, it was not for a lack of trying on the part of his employer:
Blue Ridge Paper Products, which makes the DairyPak milk carton, pleaded unsuccessfully with providers for discounts for its 5,000 covered workers. In the past five years, the company established its own clinic and pharmacy. Blue Ridge decided to try overseas healthcare after it heard that hospitals "rolled out the red carpet" to American patients based on news reports and personal accounts from a North Carolina medical traveler brought in by IndUShealth.According to the transcript from a Marketplace interview Mr. Garrett, despite the quote above about his company "dropping the ball", probably feels he isn't being treated well by the USW:
I can understand the liability concerns expressed. I also have other problems with this as well. Patients who I know that have had rotator cuff repair require several weeks of physical therapy. I personally would feel very put out if a patient had gone overseas for the procedure but I was the orthopedist back home who was asked to supervise the rehabilitation and deal with any complications that may develop. Most assuredly I would think twice about assuming care of this patient had things gone wrong with the cholecystectomy. It would also be easier to serve papers on a local physician involved with taking care of the complication, rather than finding a process server in Bangalore. |ASHLEY MILNE-TYTE: Carl Garrett is 60. He's worked as a technician at the same paper mill in North Carolina for 40 years. When I first spoke to him he was a week away from having his gall bladder removed and a rotator cuff mended at the Apollo Hospital in New Delhi.
GARRETT: "I'm not nervous. Matter of fact, I'm just excited and anxious to get going."
His employer, Blue Ridge Paper, can save tens of thousands of dollars if an employee has an operation in India rather than North Carolina. But their nascent healthcare option saves Garrett money too. The luxury package to India is completely covered by the company: he'll even get a portion of their savings. To have both operations done at home, he says, he'd fork out up to $10,000 in deductibles and out-of-plan costs.......
....Still, Carl Garrett says he can't wait that long. Instead of two free operations in India, he says he'll have to borrow the money to have them done at home.
CARL GARRETT: I'm still in a, kind of a state of disbelief. It's a crying shame that, uh, I don't have that option, simply because of a union that I have supported for 40 years. And as far as I'm concerned they have taken money out of my pocket." The irony, he says, is that the other union members he works with couldn't wait for him to get back, to decide whether to sign up for an overseas operation themselves.
Tuesday, October 10, 2006
From today's New York Times: The Last Word on the Last Breath:
The patient, only 35, had been in a persistent vegetative state for 15 years. Recently, he had developed septic bedsores and pneumonia. His kidneys were failing, and despite the feeding tube, he was losing weight. Now he was in cardiac arrest. He was dying.
But the young staff doctor had no choice. The patient's relatives, convinced that the man could communicate, had insisted that all revival efforts be made. So the doctor gave the patient a few mouth-to-mouth breaths, climbed on the bed and began vigorous chest compressions, trying cardiopulmonary resuscitation.
The patient was intubated, shocked with electric paddles and injected with epinephrine. Blood spurted as a central line was inserted into the large vein in his groin to administer medicine and fluids. EKG electrodes were placed on his arms and legs: streams of paper spilled over the floor, as the hospital room filled with people and shouted orders.
After 15 minutes, the doctors called the time of death.
"Kneeling on that bed, doing CPR, felt not only pointless, but like I was administering final blows to someone who had already had a hard enough life," said the doctor, Daniel Sulmasy, now a New York internist, medical ethicist and Franciscan friar, recalling this experience from his internship. "Why was I forced to crack this person's ribs? Why couldn't we have let the patient die in peace?"
It comes down to medical futility versus the "desire to do everything":
Many doctors believe that their medical judgment about whether CPR will be effective in a given patient's case, and their knowledge of the havoc it can wreak on a dying body, should prevail. But a patient's representative, who is often a relative, may believe that every medical option should be exercised and that a miracle could be just a chest compression away. And patients' families, spurred on by TV medical dramas, often mistakenly believe that CPR is almost always effective - a notion emphatically disproved by studies.The article cites a 1996 New England Journal of Medicine article about the unreality surrounding codes on TV. Here it is, Cardiopulmonary Resuscitation on Television - Miracles and Misinformation:
Background Responsible, shared decision making on the part of physicians and patients about the potential use of cardiopulmonary resuscitation (CPR) requires patients who are educated about the procedure's risks and benefits. Television is an important source of information about CPR for patients. We analyzed how three popular television programs depict CPR.
Methods We watched all the episodes of the television programs ER and Chicago Hope during the 1994-1995 viewing season and 50 consecutive episodes of Rescue 911 broadcast over a three-month period in 1995. We identified all occurrences of CPR in each episode and recorded the causes of cardiac arrest, the identifiable demographic characteristics of the patients, the underlying illnesses, and the outcomes.
Results There were 60 occurrences of CPR in the 97 television episodes - 31 on ER, 11 on Chicago Hope, and 18 on Rescue 911. In the majority of cases, cardiac arrest was caused by trauma; only 28 percent were due to primary cardiac causes. Sixty-five percent of the cardiac arrests occurred in children, teenagers, or young adults. Seventy-five percent of the patients survived the immediate arrest, and 67 percent appeared to have survived to hospital discharge.
Conclusions The survival rates in our study are significantly higher than the most optimistic survival rates in the medical literature, and the portrayal of CPR on television may lead the viewing public to have an unrealistic impression of CPR and its chances for success. Physicians discussing the use of CPR with patients and families should be aware of the images of CPR depicted on television and the misperceptions these images may foster.
How did these shows paint a misleading picture? Let us count the ways:
First, these three television programs give a misleading impression about the kind of people most commonly given CPR. On television, children, teenagers, and young adults accounted for 65 percent of the patients given CPR. Of the total number of deaths on the programs, 83 percent were of nonelderly patients. In fact, cardiac arrest is much more common in the elderly than in children or young adults.The reality:
Second, cardiac arrest on television was often due to acute injury, the result of gunshot wounds, motor vehicle accidents, or near-drowning; only 28 percent of the patients had primary cardiac arrests. In real life, 75 to 95 percent of arrests result from underlying cardiac disease.
Third, CPR succeeded more frequently on television than in the real world as reflected in the medical literature. On all three shows combined, 75 percent of the patients were alive immediately after their cardiac arrests, and 67 percent appeared to survive in the long term. On Rescue 911, which focuses on the successes of emergency services, the survival rate after CPR was 100 percent. Of the patients on ER, 65 percent survived the initial arrest; three of these patients died before discharge from the hospital. On Chicago Hope, 64 percent of the patients given CPR initially survived cardiac arrest, and 36 percent survived to discharge.
Rates of long-term survival after cardiac arrest as reported in the medical literature vary from 2 percent to 30 percent for arrests outside a hospital, and from 6.5 percent to 15 percent for arrests that take place inside a hospital. For average elderly patients, the rate of long-term survival after cardiac arrest outside a hospital is probably no better than 5 percent. For arrests due to trauma, the reported survival rates vary from 0 to 30 percent. Clearly, the rates on television are significantly higher than even the most favorable data reported in the literature.The role of physicians and family members varies by state:
New York is one of the few states with a law that directly addresses resuscitation orders. In New York, even when a doctor believes that CPR would be medically futile, if the patient is incapable of indicating a preference for or against it and the patient's designated representative insists it be performed, the physician must ultimately go to court to prevail. Texas, which has a complex advance directive law that includes checks and balances, ultimately sides with physicians, immunizing them from litigation.The article touches on the history of codes:
Hawaii passed legislation this year giving great weight to a patient's "comfort care" document, which specifies the patient's preferences in dire medical situations. Nonetheless, if the patient has indicated no resuscitation but the provider's own conscience dictates otherwise, a medical professional may override the document.
In New York, doctors at one hospital had a casual way of indicating to staff, without informing families, which patients should not be resuscitated : purple stickers were affixed to their charts. Occasionally, stickers were placed on the wrong charts or fell off. After these and other stories came to light, New York passed a law in 1987 that addressed the conditions under which a physician could write a D.N.R. order. Patient consent was essential.Inability of communication and the inabliity of families to accept the futility of the situation leads to half-assed exercises such as these:
The statute did say that if resuscitation was "medically futile" and no representative could be found to consent to the D.N.R. order, a doctor could write one, if another doctor also signed it. Under these narrow circumstances, a doctor's judgment that CPR would be useless was sufficient. But what if a "medically futile" patient's decision-maker insisted that CPR be performed anyway? Could a doctor's judgment prevail?
In 2003, an upstate New York hospital, seeking policy guidance, put the question to Attorney General Eliot Spitzer. Mr. Spitzer interpreted the state law to mean that even in these cases, a doctor could not enter a D.N.R. order over the objections of a family. A doctor's only recourse was to proceed to mediation, and then, if necessary, to court.
"We have gone from one extreme to the other," said Dr. Kenneth Prager, chief of medical ethics at New York-Presbyterian/Columbia, "from physicians making unilateral decisions to the situation where the family and the patient have all control."
At the same time the New York statute was being enacted, stories around the country emerged of doctors going through the motions of a code for the benefit of a family. Hospital slang like "slow code"(to suggest a leisurely walk to the bedside), "Hollywood code" (in deference to TV hospital programs) or "light blue code" (an allusion to code blue, the term for a cardiac arrest resuscitation) became public.Dr. Nic describes the origins of CPR:
In 1960 JAMA published an article titled "Closed-Chest Cardiac Massage." It was based on 5 (yes 5) case reports about acute cardiopulmonary arrest. It concluded that cardiac massage was proven to be effective. This was the birth of CPR. In 1993 the Journal of the American Board of Family Practice did a 30 year review of in-hospital CPR. Of the 19,955 patients in the study 15% survived.And also decribes more code buffonery:
From a treatment perspective, it is the last one DNI but not DNR that poses a severe problem. We can do every part of the resuscitation process except put in a breathing tube. In order to perform CPR/recuscitate a person the first step is securing the airway, i.e. intubation. No amount of chest compressions to move the blood through the body will do any good if the blood has no oxygen to carry. Even if a person is young enough to get a blood pressure and pulse back, their brain has been deprived of oxygen.I wholeheartedly agree. IMHO DNI but "full code", "shock only", "chemical code" orders are in a word, b.s. And as far as that goes:
In my mind this is doing a patient harm. I in good conscience could not fill out the paperwork to make a patient DNI but not DNR. And to be honest, I view my colleagues who do so with much less respect as physicians.

The "B" and "C" do little good for the patient without the "A". When we engage in "Hollywood codes", "slow codes", or "light blue codes" we are treating the families, not the patient. When we know better.
See Kevin's take on this here |
Sunday, October 08, 2006

Georgia 33 Tennessee 51
It was fun while it lasted. Georgia was exposed this weekend for all to see (as was Auburn). Two winnable conference games coming up before the Worlds Largest Outdoor Cocktail Party. |
Sunday, October 01, 2006

Georgia 14 Ole Miss 9
Gotta get some offense befrore the Vols come to Athens on Saturday. JT3 to start? Maybe. |
That won't gross out out. Take a different look at the surroundings On Location With Rick Lee: The O.R. |





