Wednesday, October 25, 2006
From this month's Annals of Surgery the march of the specialty of "acute care surgery" moves on. An Acute Care Surgery Model Improves Outcomes in Patients With Appendicitis:
Objective: To compare outcomes of appendectomy in an Acute Care Surgery (ACS) model to that of a traditional home-call attending surgeon model.
Summary Background Data: Acute care surgery (ACS, a combination of trauma surgery, emergency surgery, and surgical critical care) has been proposed as a practice model for the future of general surgery. To date, there are few data regarding outcomes of surgical emergencies in the ACS model.
Methods: Between September 1999 and August 2002, surgical emergencies were staffed at the faculty level by either an in-house trauma/emergency surgeon (ACS model) or a non-trauma general surgeon taking home call (traditional [TRAD] model). Coverage alternated monthly. Other aspects of hospital care, including resident complement, remained unchanged. We retrospectively reviewed key time intervals (emergency department [ED] presentation to surgical consultation; surgical consultation to operation [OR]; and ED presentation to OR) and outcomes (rupture rate, negative appendectomy rate, complication rate, and hospital length of stay [LOS]) for patients treated in the ACS and TRAD models. Questions of interest were examined using χ2 tests for discrete variables and independent sample t test for comparison of means.
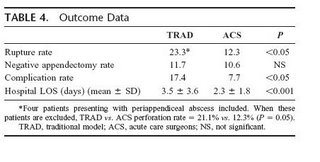
Results: During the study period, 294 appendectomies were performed. In-house ACS surgeons performed 167 procedures, and the home-call TRAD surgeons performed 127 procedures. No difference was found in the time from ED presentation to surgical consultation; however, the time interval from consultation to OR was significantly decreased in the ACS model (TRAD 7.6 hours vs. ACS 3.5 hours, P < 0.05); negative appendectomy rates were similar. The complication rate in the ACS model was decreased (TRAD 17.4% vs. ACS 7.7%, P < 0.05), as was the hospital LOS (TRAD 3.5 days vs. ACS 2.3 days, P < 0.001). Conclusions: In patients with acute appendicitis, the presence of an in-house acute care surgeon significantly decreased the time to operation, rupture rate, complication rate, and hospital length of stay. The ACS model appears to improve outcomes of acute appendicitis compared with a TRAD home-call model. This study supports the efficacy and efficiency of the ACS model in the management of surgical emergencies.
So having the in-house attending decreased ER time (elimnate those boarders), decreased rupures and complications, and decreases length of stay. All good things, no?
The "why" of acute care surgery is explained:
The future of trauma surgery as a career has become a topic of much debate in academic circles. Many factors have likely contributed to the relative shortage of trauma critical care surgeons. One recurring theme noted by a number of authors is the decreasing operative exposure for surgeons caring for injured patients. The predominance of nonsurgical management in blunt trauma and the decreasing incidence of penetrating trauma have resulted in a decreased operative experience in recent years. At the same time, emergency care is at a crisis, with widespread problems of access, overcrowding, boarding, and delays. Marked increases in emergency department visits by older, sicker patients, many with surgical emergencies, are more common and require a continuous workforce of surgical specialists to respond, evaluate, operate, and deliver critical care. Unfortunately, emergency departments are having significant and greater difficulties assuring specialist coverage. One recent report documents that over two thirds of emergency department directors report shortages of on-call specialists at their hospitals.
In response to these issues, many hospitals have had their trauma programs absorb emergency surgery into their practice.3,7 This model of acute care surgery (ACS), a combination of trauma surgery, broad-based emergency surgery, and surgical critical care, has been championed by the American Association for the Surgery of Trauma and a number of other trauma and surgical societies.2 A formal training curriculum is being developed, and plans for potential board certification are being explored. Several programs have reported their experience with the integration of emergency general surgery into their trauma programs. Most of these reports focus on surgeon satisfaction, surgeon caseload and diversity, and surgeon productivity. None, to date, has examined the effect of this integrated model on outcomes for patients with nontrauma surgical emergencies.
Here is a table of the timing data:
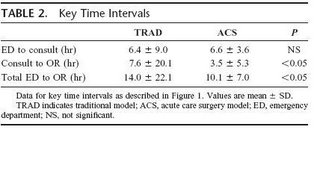
So the ACS group cut the consult to OR time by half, and the ED to OR time by almost a third. Here are some more figures with their accompanying text:
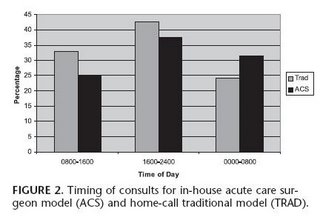

Surgical consultation occurred most frequently between 1600 and 2400 in both groups (Fig. 2). More than 30% of consultations in the ACS group occurred between 0000 and 0800. In contrast, more than 30% of consultations in the TRAD group occurred between 0800 and 1600. The timing of operative intervention is presented in Figure 3. More than 40% of surgeries in the TRAD group occurred between 1600 and 2400. In contrast, more than 40% of surgeries in the ACS group occurred between 0000 and 0800, compared with only 25% of surgeries in the TRAD group (P = 0.08). Of note, laparoscopic appendectomy was performed in only 10% of the ACS group and 6.5% of the TRAD group (P = not significant). One patient in each group required conversion to an open procedure
The results summarized:
Here is the discussion, emphasis is mine:
Caring for patients with surgical emergencies is one of the cornerstones of our profession. The potential to promptly diagnose an acute surgical problem and intervene in a timely fashion presents the surgeon with a unique opportunity to immediately impact a critically ill patient. As the population ages, the patients with surgical emergencies tend to have considerably more comorbid conditions and active medical problems. Unfortunately, these patients present at all hours of the day and night. They are challenging, time-consuming, and disruptive to the busy practicing surgeon. As a result, the surgeon's well-orchestrated and extremely efficient schedule of the day (outpatient office hours, elective surgical caseload, and for some, protected academic time) is often greatly disrupted by an emergent consultation. When emergent surgery is necessary, identifying available time in a busy OR schedule that does not further impact the surgeon's other responsibilities may be an additional challenge. Compounding this, many emergencies seem to occur on off hours and weekends, disrupting rest, family, and personal times. The possibility of being up all night or all weekend has both explicit and implicit effects on surgeons scheduling full clinical loads the following day. Finally, very little recognition or value can be currently found in academic surgical departments for taking on this difficult and complex patient population. Traditionally, the surgical trainee has played a major role in patient care during off hours. While the educational experience offered by this period of relative nonsupervision may be significant, the care rendered to those patients with surgical emergencies (arguably the ones who can least afford suboptimal or minimally supervised care) may be less than ideal. In many instances, faculty are only in phone contact with surgical trainees regarding emergent care of an acutely ill patient. Even at the academic medical center, the sickest emergency patient may not see a faculty surgeon for many hours during the crucial initial phases of emergency surgical care.
The acute care surgeon may be an answer to many of these and other issues prevalent in the current surgical setting. The backbone of such a program, the trauma and critical care surgeon, is already present at many medical centers. Seventy percent of level I trauma centers currently have 24/7 in-house faculty trauma surgeons.1 Because of the broad nature of injury, this specialty is already trained and familiar with a wide scope of surgical problems. In addition, more than 75% are trained and practice critical care so they have an expertise in the management of the comorbid conditions so often present in the emergent surgical patient. Expanding the trauma surgeon's role to a broader surgical emergency one has already begun to occur at a number of hospitals where emergency general surgery has been added to the responsibilities of the trauma surgeon. This new acute care surgeon can be at the bedside of the patient with a surgical emergency at a moment's notice. The experience that they bring to the bedside at all hours of the day and night should be beneficial to both the care of the ill surgical patient as well as the education of the surgical trainee.
Since this paper was presented at a meeting, the audience was able to ask questions. This one sums up, IMHO, the matter best:
Dr. Mark A. Malangoni (Cleveland, Ohio): Dr. Schwab, I certainly enjoyed your presentation and enjoyed reading the paper as well. This morning President Pellegrini alluded to the evolution of acute care surgery as a new surgical subspecialty, and you have presented high quality data that this model works in the care of a common surgical disease, acute appendicitis. The 4-hour reduction in time from the consultation to the operating room translates to a 47% risk reduction in rupture and a 56% risk reduction in complications as well as a one-day-shorter hospital stay, improvements that are hard to argue with.
If I was an acute care surgeon contemplating the importance of this new subspecialty, I would say these data unquestionably support the development of this new discipline. As a general surgeon, I would look at the data differently and I would conclude that it confirms that the existing information that reducing the delay from the time of diagnosis to the operating room in adults results in better outcomes, a fact that has been certainly supported by many previous studies as well as your current study. This strongly suggests that it is quality patient care, not surgeon convenience, that must take precedence.
I have a couple of questions for you. You have already addressed the issue of patient presentation at the emergency department and its potential impact. My 2 questions are: The acute care surgeons seem to get a greater number of consults between midnight and 8:00 am. Do you think the fact that the emergency medicine physicians knew that there was an in-house attending surgeon that would respond to consultation resulted in a propensity for them to call you and hence may have decreased the time to consultation for the acute care surgeon and may have affected the results?
Second, we all know that this acute care surgery model is still controversial, particularly in nonteaching hospitals, where there are fewer surgical subspecialists. Now, if you believe that all hospitals should have acute care surgeons, could you expand a bit upon how that would occur? If you feel that this is a model that only should apply to those of us who work in teaching hospitals where there may be a greater number of surgical subspecialists, what should be done in the community hospitals where there is less likely to be a trained acute care surgeon present?
The highlighted quote reminds me of a summary post of another paper that the greatest advantage of the acute care surgeon was seen by the "somnolent elective surgeon". The reply:
Dr. C. William Schwab (Philadelphia, Pennsylvania): First of all, I don't know if the Yogi Berra element was in work here. And that is, you know, showing up is 89% of the game. I just don't know if that was true.
I will tell you that the way the emergency physicians consulted the surgical service did not change whether it was a month in which the acute care surgery model was in place or the traditional model was in place. The consults came to a third-year surgical resident, he responded, sought consultation if necessary from a more senior surgical resident and at that point we were brought in, meaning the faculty. The fact that we were there, I just can't say. And as I said but didn't explain it, I wish this was a time-in-motion study in which I could provide you all hour to hour what was going on in the management of these cases. I can't. And this is really looking at that from really, I think, 37,000 feet.
The next question you asked is, do I think this is a model that works only in a teaching hospital? For me to speculate on that is looking into a crystal ball. I will tell you that I have 2 colleagues that are in trauma critical care, both of whom have been recruited from academic surgery into the community practice and specifically hired by hospitals with the consent, approval and support of the departments of surgeries in these community hospitals to establish an acute care surgical model to relieve them of all the burden of the ED and the trauma patients.
It is an interesting observation. I personally do not think that this model is only for the academic medical centers or teaching hospitals. I think it is applicable to any particular hospital. I also don't think it is applicable only for surgeons that have special training in critical care and experience in trauma. I think any general surgeon broadly based and well trained with an interest can be an acute care surgeon. I think we ought to design to train the future generations with the curriculum that the AAST is developing, but we need to stay tuned for what that looks like.
The acute care surgeon concept benefits the hospital by having a group of dedicated surgeons who will respond to the emergency room. It benefits the interested surgeon because it allows for regularity of schedule. With specialist coverage of ED's becoming an increasing problem, and the regulated schedules of current trainees I believe that over time this model will become more widespread and accepted. I know that my colleague in the Rocky Mountains may disagree.
Now in my last post on this subject I did not mean to imply that those who enjoyed surgery, but did not pursue a residency were lazy, but that in my experience those who left my training program were discontents which were best described as "lazy". I think that even if "surgical hospitalists" become more prevalent, that "part-time" training won't catch on. This is a solution in search of a problem now, but maybe not a few years ago. Look at how surgery has fared in the match over the past few years: (click to enlarge)

What changed between 2002 and 2003? Workhour limits. So the "lifestyle sensitive" have started to join up.
Labels: appendicitis, Future of Surgery
|





