Monday, October 16, 2006
Send the Whirlybird III....
Catching up on my reading I found this in the June issue of The Journal of Trauma:Helicopter Scene Transport of Trauma Patients with Nonlife-Threatening Injuries: A Meta-Analysis:
What they did was analyze the above studies to determine if, based on objective criteria, patients would benefit from a helicopter transport. For those not familiar with the criteria here is an explanation:
Not all of those scoring systems were used in all of the studies so the ISS, TS, and TRISS were evaluated. The severity criteria were as follows:
So, looking at the first set of data:
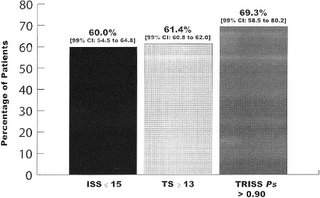
As you see the range of patients with an ISS at or below 15 ranges from 85.1 percent to 34.6 percent, with a mean of 60 percent. So by this reckoning, sixty percent of these patients did not have an injury severity high enough to justify helicopter transport. Moving along:
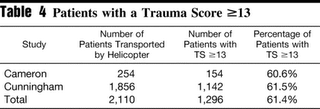
Three studies used the trauma score as the criteria. All had over sixty percent of their patients with a trauma score greater than 13. So, by their criteria, only fort percent of the patients required helicopter transport. This appears consistent with the results above.
Here the TRISS is examined. A patient with a P> 90 has a greater than 90 percent chance of survival, and should not require helicopter transport. The percentage ranges from 41.9 to 90 percent with an average of 69.3 percent. So by this criteria almost 7 out of 10 patients should not have required helicopter transport.
This is the "what, no helicopter ride home?" group. The percentages here are not as large, perhaps due to the "non-standard" criteria.
Here is a comparison of the "minor injuries" based on scoring system. They seem to compare well.
So why are all of these patient's riding the whirlybird? The authors opine:
There are concerns about helicopter safety:
The authors provide an explanation for the change in the results of the studies:
So the old struggle of overtriage/undertriage strikes again. Field decisions are made based on physiologic status and mechanism of injury (MOI). MOI can overestimate severity, and can be overly sensitive. I myself believe that helicopter transport is overutilized and some restraint would be helpful from time to time.
See also:
Send the Whirlybird
Send the Whirlybird II |
Catching up on my reading I found this in the June issue of The Journal of Trauma:Helicopter Scene Transport of Trauma Patients with Nonlife-Threatening Injuries: A Meta-Analysis:
Background: Helicopters have become a major part of the modern trauma care system and are frequently used to transport patients from the scene of their injury to a trauma center. While early studies reported decreased mortality for trauma patients transported by helicopters when compared with those transported by ground ambulances, more recent research has questioned the benefit of helicopter transport of trauma patients. The purpose of this study was to determine the percentage of patients transported by helicopter who have nonlife-threatening injuries.
Methods: A meta-analysis was performed on peer-review research on helicopter utilization. The inclusion criteria were all studies that evaluated trauma patients transported by helicopter from the scene of their injury to a trauma center with baseline parameters defined by Injury Severity Score (ISS), Trauma Score (TS), Revised Trauma Score (RTS), and the likelihood of survival as determined via Trauma Score-Injury Severity Score (TRISS) methodology.
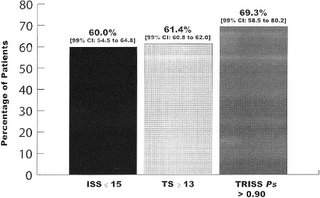
Results: There were 22 studies comprising 37,350 patients that met the inclusion criteria. According to the ISS, 60.0% [99% confidence interval (CI): 54.5-64.8] of patients had minor injuries, According to the TS, 61.4% (99% CI: 60.8-62.0) of patients had minor injuries. According to TRISS methodology, 69.3% (99% CI: 58.5-80.2) of patients had a greater than 90% chance of survival and thus nonlife-threatening injuries. There were 25.8% (99% CI: -1.0-52.6) of patients discharged within 24 hours after arrival at the trauma center.
Conclusions: The majority of trauma patients transported from the scene by helicopter have nonlife-threatening injuries. Efforts to more accurately identify those patients who would benefit most from helicopter transport from the accident scene to the trauma center are needed to reduce helicopter overutilization.
What they did was analyze the above studies to determine if, based on objective criteria, patients would benefit from a helicopter transport. For those not familiar with the criteria here is an explanation:
The ISS is an anatomic scoring system for patients with multiple injuries and does not include physiologic variables. The ISS ranges from 0 to 75 with the severity of injury and mortality increasing with the score. Patients with an ISS >15 are deemed to require specialized trauma care while patients with an ISS of 15 or less are considered to have nonlife-threatening injuries. The original TS included four physiologic parameters (respiratory rate, respiratory expansion, systolic blood pressure, capillary refill) and the Glasgow Coma Scale (GCS). It had a range from 1 to 16 points. Patients with a score of 12 or less were deemed to be seriously injured and required specialized trauma care. The TS was revised in 1989 and became the RTS. Two of the physiologic parameters (respiratory expansion and capillary refill) were dropped. The range of the RTS is 0 to 12. Patients with a score of 11 or less are deemed to require specialized trauma care. While the RTS is most commonly used in the prehospital setting, a weighted form of the scale is used to predict patient outcomes following trauma. With the weighted RTS, greater emphasis is placed on the GCS. The range for the weighted RTS is 0 to 7.8408. Higher scores are associated with a better prognosis. Patients with a weighted RTS score of <4 are felt to benefit from specialized trauma care while patients with a score of ≥4 are generally considered to have minor injuries. The TRISS system combines the RTS, the ISS, the patient's age, and the type of trauma sustained (blunt or penetrating) to determine a probability of survival (P s)
Not all of those scoring systems were used in all of the studies so the ISS, TS, and TRISS were evaluated. The severity criteria were as follows:
To determine which patients were unlikely to benefit from helicopter transport, we used the standard trauma scoring systems described above. Based upon validated criteria, patients having a TS ≥13, a RTS >11, a weighted RTS ≥4, and/or an ISS ≤15 were deemed to have sustained nonlife-threatening injuries and therefore did not require helicopter transport. Likewise, a TRISS-derived probability of survival (P s) of greater than 0.90 (a 90% or better chance of survival) also represents nonlife-threatening injuries and was included as one of the inclusion criteria. Finally, patients who were discharged from the emergency department or hospital within 24 hours of admission for trauma are generally considered to have nonlife-threatening injuries and were included in the inclusion selection criteria.
So, looking at the first set of data:
As you see the range of patients with an ISS at or below 15 ranges from 85.1 percent to 34.6 percent, with a mean of 60 percent. So by this reckoning, sixty percent of these patients did not have an injury severity high enough to justify helicopter transport. Moving along:
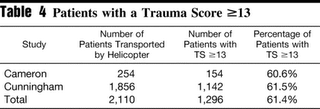
Three studies used the trauma score as the criteria. All had over sixty percent of their patients with a trauma score greater than 13. So, by their criteria, only fort percent of the patients required helicopter transport. This appears consistent with the results above.
Here the TRISS is examined. A patient with a P> 90 has a greater than 90 percent chance of survival, and should not require helicopter transport. The percentage ranges from 41.9 to 90 percent with an average of 69.3 percent. So by this criteria almost 7 out of 10 patients should not have required helicopter transport.
This is the "what, no helicopter ride home?" group. The percentages here are not as large, perhaps due to the "non-standard" criteria.
Here is a comparison of the "minor injuries" based on scoring system. They seem to compare well.
So why are all of these patient's riding the whirlybird? The authors opine:
Our study demonstrated that the majority of trauma patients transported by medical helicopter from the scene had nonlife-threatening injuries. We believe there are two possible explanations for this phenomenon. First, there may be a significant degree of overutilization of helicopter scene flights for trauma by air-medical services despite quality assurance oversight that reveals these flights to be nonbeneficial. Second, and more probable, the apparent overutilization may be because of a significant degree of overtriage in the field by prehospital providers resulting in inappropriate requests for helicopter scene transport.
There are concerns about helicopter safety:
There has been a marked increase in the number of medical helicopter accidents in the United States. In fact, half of all accidents in one 10-year study (1993-2002) occurred during the last 3 years of the study period. Because of the lack of a centralized database, it is impossible to determine whether this increase in accidents reflects a decline in operational safety or merely reflects the fact that there are more aircraft flying more missions. In January of 2005, in response to a sharp increase in fatal medical helicopter accidents, the NTSB and the Federal Aviation Administration (FAA) launched safety reviews of medical helicopters.
The authors provide an explanation for the change in the results of the studies:
It is curious that early studies demonstrated that helicopter transport decreased mortality from trauma while more recent studies have indicated little or no benefit from helicopter transport. The authors believe this reflects the tremendous improvements in ground prehospital care observed over the last 20 years including more widespread advanced life support units and markedly enhanced EMT and paramedic education. Other factors that may explain this difference include improved categorization of hospitals, the organization and implementation of regional trauma systems, trauma centers, and postgraduate educational programs that specialize in trauma care.The authors then list the limitations of the study, the last IMHO is the most relevant (emphasis mine)
Fourth, current helicopter utilization criteria are applied at the scene of trauma while the ISS is calculated retrospectively once the patient has received definitive care. The use of the ISS has been reported to not identify a subset of trauma patients who may benefit from definitive trauma care. However, the ISS is usually applied retrospectively following hospital admission and is not routinely used for prehospital trauma triage decision making. The ISS is the scoring system most commonly used in the studies referenced in this article.
The use of the TRISS system has both benefits and limitations. TRISS is widely used and validated. However, it is applied retrospectively and does not aid prehospital personnel in determining which patients may actually benefit from helicopter transport. Furthermore, the TRISS has been reported to overestimate survival in patients who are severely injured. However, in our cohort we were interested in patient with minor injuries.
So the old struggle of overtriage/undertriage strikes again. Field decisions are made based on physiologic status and mechanism of injury (MOI). MOI can overestimate severity, and can be overly sensitive. I myself believe that helicopter transport is overutilized and some restraint would be helpful from time to time.
See also:
Send the Whirlybird
Send the Whirlybird II |






