Monday, December 26, 2005
More on Dr. Shanthaveerappa.....
UPDATE: Welcome, participants of the Skeptic's Circle Check out these other posts about Dr. Shanthaveerappa.
From the AJC:Cancer doctor loses his license
Back when Dr. Kevorkian first started making news I thought it odd that a pathologist would be offering such a "service". I would have thought that the "poster boy" for physician assisted suicide would have been a physician that had contact with live patients. From reviewing his CV Dr. Shantha appears to have no formal training in oncology. I wonder how many of his patients knew that?
According to an Atlanta news station Dr. Shantha will hold a press conference after his arraignment. |
UPDATE: Welcome, participants of the Skeptic's Circle Check out these other posts about Dr. Shanthaveerappa.
From the AJC:Cancer doctor loses his license
doctor charged with injecting cancer patients with weedkiller and defrauding insurance companies had his license suspended Friday morning.Regardless of how one feels about Dr. Shanthaveerappa's treatments, what has brought this out was alleged insurance fraud:
People who say that Dr. Totada R. Shanthaveerappa saved their lives continued to rally to his defense Friday afternoon, even as two questionable patient deaths came to light.
The Georgia Medical Board of Examiners, after an emergency meeting, voted 9-0 to recommend the suspension of Shanthaveerappa's license. He was given notification of the suspension at his Stockbridge clinic, said Dr. Jim McNatt, the board's medical director.
An 87-count federal indictment accuses Shanthaveerappa, 70, also known as T.R. Shantha, of treating patients with drugs not authorized by the U.S. Food and Drug Administration, then falsely billing insurance companies by saying he had used approved drugs. The indictment says Shanthaveerappa used dinitrophenol, or DNP, a weedkiller and insecticide, and Ukrain, which is not approved for use in the United States.And while Dr. Shanthaveerappa has his defenders, other allegations are beginning to surface:
Pierce's lawyer, Michael J. Hannan III, said Pierce, a musician and songwriter from Tennessee who sang and played in Juice Newton's band in the 1980s, was diagnosed with cancer in his tonsils in February 2004. The tumor was removed, and Pierce was told by his doctor to get chemotherapy and radiation treatment. But Pierce chose not to do so, because it could have ruined his voice..."they don't like him at this hospital".... I wonder why?
Pierce sought out alternative therapies on the Internet and found Shanthaveerappa, who has several Web sites, including Wehealcancer.org. According to the lawsuit, Pierce went to Stockbridge and gave Shanthaveerappa a cashier's check for $40,000.
According to the suit, Pierce was placed into a heat chamber where his blood was to be heated to 106 degrees. "Mr. Pierce was advised that this would kill the cancer," the suit says. He was also given intravenous injections.
The suit gives this description of what happened next:
On April 18, 2004, after three weeks of therapy, Pierce had a high fever, uncontrollable shakes and severe abdominal pain. He called a nurse from Shanthaveerappa's office, who drove him to the Henry Medical Center. The nurse told Pierce not to tell hospital officials he was seeing Shanthaveerappa, because "they don't like him at this hospital." He was transferred to Emory Medical Center, where he was operated on.
"They found he had a raging infection in his abdomen," Hannan said in an interview Friday. Pierce also had aplastic anemia. Surgeons removed his colon, and he later received a colonostomy.
Hannan said Shanthaveerappa treated Pierce with low-dose chemotherapy, not enough to stop the cancer but enough to weaken his immune system and allow infection to spread.
"His immune system was completely compromised. Shantha's treatment gave him false hope. It didn't give him the chance conventional treatment would have."
Back when Dr. Kevorkian first started making news I thought it odd that a pathologist would be offering such a "service". I would have thought that the "poster boy" for physician assisted suicide would have been a physician that had contact with live patients. From reviewing his CV Dr. Shantha appears to have no formal training in oncology. I wonder how many of his patients knew that?
According to an Atlanta news station Dr. Shantha will hold a press conference after his arraignment. |
Saturday, December 24, 2005
Merry Christmas....

From the second chapter of the Gospel of Luke:
Best wishes for you and your family this holiday. |

From the second chapter of the Gospel of Luke:
And it came to pass in those days, that there went out a decree from Caesar Augustus, that all the world should be taxed. (And this taxing was first made when Cyrenius was governor of Syria.)
And all went to be taxed, every one into his own city. And Joseph also went up from Galilee, out of the city of Nazareth, into Judea, unto the city of David, which is called Bethlehem (because he was of the house and lineage of David), to be taxed with Mary his espoused wife, being with child.
And so it was, that, while they were there, the days were accomplished that she should be delivered. And she brought forth her firstborn son, and wrapped him in swaddling clothes, and laid him in a manger; because there was no room for them in the inn.
And there were in the same country shepherds abiding in the field, keeping watch over their flock by night. And lo, the angel of the Lord come upon them, and the glory of the Lord shone round about them: and they were sore afraid.
And the angel said unto them, "Fear not: for, behold, I bring you good tidings of great joy, which shall be to all people. For unto you is born this day in the city of David a Savior, which is Christ the Lord. And this shall be a sign unto you; Ye shall find the babe wrapped in swaddling clothes, lying in a manger."
And suddenly there was with the angel a multitude of the heavenly host praising God, and saying, "Glory to God in the highest, and on earth peace, good will toward men."
Best wishes for you and your family this holiday. |
Friday, December 23, 2005
Almost Heaven....
One of the great things about Grand Rounds is the exposure to health care blogs that I may not read on a regular basis. One is the Health Care Law Blog. Personally notable not only for the subject matter, but also because Mr. Coffield lives and works in Charleston, West Virginia. A city where I had the privilege to spend some of my formative years. But all is not well in the Kanawha Valley these days. From The Charleston Gazette:CAMC expects doctors on call
One of the great things about Grand Rounds is the exposure to health care blogs that I may not read on a regular basis. One is the Health Care Law Blog. Personally notable not only for the subject matter, but also because Mr. Coffield lives and works in Charleston, West Virginia. A city where I had the privilege to spend some of my formative years. But all is not well in the Kanawha Valley these days. From The Charleston Gazette:CAMC expects doctors on call
Seven heart surgeons who boycotted Charleston Area Medical Center General Hospital’s trauma center Monday will still get called in and are expected to show up if needed, hospital officials said Thursday.Nothing new there, I'm afraid. There was a cardiopulmonary bypass pump at the Gen Div, but I don't recall ever using it during my tenure. We always did what we could, and transferred the patients to Memorial of they needed the heart guys. As usual, money comes into the picture:
The surgeons’ lawyer, Karen Miller, said the doctors won’t show up.
“They are sticking by it until they get their operating room because they feel they have to for patient safety,” she said.
The surgeons say the current facilities at General’s trauma unit are dangerous to patients, and have told the hospital they will not report to the trauma unit when called until administrators give them the equipment and trained staff they need to perform surgeries safely.
Hospital officials say the trauma center is safe, and the surgeons are upset because they don’t get as much pay as other doctors when they are on call for the center.The heart guys were involved very rarely in the care of the trauma patient
In 2004, of the 2,557 trauma patients at CAMC, one patient was admitted for heart treatment, according to information from the National Trauma Data Bank maintained by the American College of Surgeons. The trauma center consulted with heart surgeons only 12 times that same year.Other specialists are paid quite handsomely, but show up more often:
CAMC contends the issue is money. The doctors want $2,000 for every day they are on call, but CAMC says the doctors don’t come in enough. Furthermore, federal anti-kickback laws forbid the hospital from paying the surgeons that much for the work they put in, Witte said.After the recent struggles in West Virginia with liability issues, it's sad to see that things still haven't settled down. |
Some doctors in other fields make thousands of dollars for just being on-call for the trauma center. CAMC’s four neurosurgeons, including Schmidt, get $3,000 each day and were summoned to the trauma center 197 times and consulted 461 times in 2004, according to the trauma data bank.
The hospital’s 12 orthopedic, or bone, surgeons reported to the trauma unit 858 times and consulted 536 times that same year. Those doctors are paid $2,000 per on-call day, Witte told the Gazette in October.
Appendicitis and The CT scanner.....
A commenter to this post by the Grunt Doc has resurrected the debate over the appropriateness of CT scanning to look for appendicitis. I will repost the well-written comment:
One issue I have with this study is that the most recent data is about six years old, while the data from the above studies is much more recent. CT scanning has improved much over the past six years and the techniques for performing and interpreting these studies has improved as well. Another is that from the data, the more CT/US that was done, the rate of NA fell. Looking at the following figures:
 This represents a running percentage of NA during the study period.
This represents a running percentage of NA during the study period.
 This represents the percentage of patients who underwent CT/US during the study period. As you can see the peak usage of CT/US correlates with reduction in the rate of NA.
This represents the percentage of patients who underwent CT/US during the study period. As you can see the peak usage of CT/US correlates with reduction in the rate of NA.
And at least in my institution more than 40 percent of patients with RLQ pain are having CT/US done. Another question not answered, how many patients with "equivocal" exams were sat on and then ruptured in this study? While there is much debate on NA after CT there is little evidence that CT is missing appendicitis.
This debate will rage on, at least until studies utilizing 16 and 64 slice scanners begin to come out. For now we will have plenty to argue about. |
A commenter to this post by the Grunt Doc has resurrected the debate over the appropriateness of CT scanning to look for appendicitis. I will repost the well-written comment:
My wife, a fellow emergency physician here at Landstuhl Regional Medical Center (Germany), had a 30yo male with classic signs for appendicitis (i.e. RLQ pain, RLQ ttp, rebound, guarding) a few nights ago. After completing her Hx and PE she called the SOD (surgeon of the day) for a consult stating that she believed her patient had an acute appendicitis that required surgical intervention. The surgeon, of course, asked her what the CBC and UA results were... She stated that they were still pending.The subject of missed diagnosis lawsuits has been raised by guest-blogger Dr. Tony at Kevin MD as well as his own site. I have not heard of lawsuits arising from removing a normal appendix, but I have seen cases referred for peer review in my hospital. The patients were much like the one described above, young males with a classic presentation. At my institution the default setting seems to be to get a CT scan first and call later. If the CT is negative the patient is discharged or admitted to their PCP's for further evaluation. So not only can unnecessary operations be avoided, hospital stays for "serial exams" can be as well. The lay press is on the case as well:
The SOD went off on her questioning her reasoning for a surgical consult without the benefit of laboratory results... Taking the high road she calmly stated that the labs were pending and would be resulted shortly after his arrival to the ED. Upon his arrival he berated her in front of the entire ED staff for a premature consult. Again, taking the high road, she thanked him for arriving in the ED so quickly and directed him to the patient's bedside. Moments after examining the patient he filled out a buck slip and took the patient to the OR for his appendectomy -- the labs were still pending as he wheeled the patient to the OR...
During his tirade, the SOD told my wife that he would be interested to hear what her colleagues' positions are on calling for a surgical consult prior to labs being resulted -- keep in mind that this patient was a "classic" presentation of acute appendicitis. My response was as follows (not all references used in this informal e-mail are listed -- it was never intended for publication so please forgive any plagiarism of Tintinalli):
Per our discussion....
I believe patients with abdominal pain can be broken down into four groups:
1. Patients who demonstrate classic presentation for acute appendicitis
2. Patients with signs and symptoms that are suspicious but not diagnostic for appendicitis
3. Patients with abdominal pain in whom appendicitis is considered to be a remote diagnostic possibility
4. All high-risk special populations presenting with abdominal pain (i.e. elderly, pediatric, pregnant, immunocompromised)
When evaluating a patient in group one I believe immediate surgical consultation is appropriate... While I would draw the usual labs (i.e. CBC, UA), I would NOT wait for their results before consulting surgery. After all, surgery is going to see this patient whether their WBC count is 8 or 80. Why delay surgical evaluation when the CBC and UA results will not change your decision to have this patient evaluated by a surgeon? The patient you described to me clearly fell into group one. I believe the surgeon would agree seeing as how he took the patient straight to the OR and removed his appendix. The finding of a normal appendix during surgery, while indicative of a misdiagnosis, should NOT be considered an error in the patient's care. After all, a certain percentage of normal appendices should be removed by every general surgeon during the routine performance of their duties - cast a broad net and all... And while the historical accepted incidence of removing a normal appendix 20% of the time is no longer the gold standard due to the advances made in CT and US (Townsend: Sabiston Textbook of Surgery, 17th ed., Copyright © 2004 Saunders, An Imprint of Elsevier. P 1387), the occasional removal of a normal appendix when dealing with patients in group one is to be expected.
As for the CBC - "The WBC is of limited value. The sensitivity of an elevated WBC above 10,000/uL in acute appendicitis is 70 to 90 percent, but the specificity is very low. More important, the positive and negative predictive values of an elevated WBC in acute appendicitis are 92 and 50 percent, respectively (Vermeulen B, Morabia A, Unger PF: Influence of white cell count on surgical decision making in patients with abdominal pain in the right lower quadrant. Eur J Surg 161:483, 1995. Hoffman J, Rausmussen O: Aids in the diagnosis of acute appendicitis. Br J Surg 76:774, 1989. Marchand A, Van Lente F, Galen RS: The assessment of laboratory tests in the diagnosis of acute appendicitis. Am J Clin Pathol 80:369, 1983.)."
As for the UA "Abnormal urinalysis results, excluding proteinuria, are found in 19 to 40 percent of patients with acute appendicitis. Abnormalities include pyuria, hematuria, and bacteriuria, possibly related to the extension of appendiceal inflammation to the ureter (Kretchmar LH, McDonald DF: The urine sediment in acute appendicitis. Arch Surg 87:209, 1963. Puskar D, Bedalov G, Fridrih S, et al: Urinalysis, ultrasound analysis, and renal dynamic scintigraphy in acute appendicitis. Urology 45:108, 1995.)."
In conclusion, I agree with the immediate surgical consultation when caring for a patient that falls into group one. That is how I was trained. That is how I currently practice. That is how I will continue to practice. If the surgeon chooses to delay their evaluation until the labs are resulted then I must concede that making that decision falls within the scope of their practice. And they, of course, will then be held responsible should their decision to delay evaluation results in a poor outcome for the patient - albeit unlikely... Bottom line, however, is that an immediate surgical consult is clearly indicated in group one patients. The decision to wait for lab results and/or imaging and the ultimate decision of cut versus do not cut falls within the bailiwick of the surgeon being consulted on the case. I would have called before the labs were resulted...
END OF E-MAIL TO MY WIFE
As you may have deduced -- the patient did NOT have an acute appendicitis. I think he turned out to have a kidney stone!!!
I would be interested to hear the perspectives of other EP's out there regarding when to call for a surgical consult on patients that fit into group one (listed above)...
But recent research has questioned that tolerance of error, showing that unnecessary appendectomies are both risky and expensive. A University of Washington study found that, among adults, unnecessary appendectomies typically resulted in a six-day hospital stay, while one patient in 40 develops serious complications and 1.5 percent of the patients die.Doing a PubMed search for "appendicitis ct" gave, as expected, plenty of results. Here are just a few:Rapid CT diagnosis of acute appendicitis with IV contrast material.
Dr. David R. Flum, an assistant professor of surgery at the University of Washington in Seattle who led the 2002 study, estimates that Americans paid $741.5 million for unnecessary appendectomies on adults in 1997, the year on which his study focused.
The purpose of this study was to determine the sensitivity and specificity of computed tomography (CT) without administration of oral contrast in confirming suspected acute appendicitis. One hundred seventy-three patient studies were retrieved by a computer-generated search for the word "appendicitis" in radiology reports. Patients presenting to the emergency department over an 8-month period were examined for acute abdominal pain or suspected acute appendicitis. IV-contrast-enhanced CT scans of the abdomen and pelvis were obtained without oral or rectal contrast. Criteria for diagnosis of acute appendicitis included a dilated appendix (>6 mm), periappendiceal inflammation, or abscess. Final diagnoses were established with surgical/clinical follow-up, histopathological analysis or both. The standard time (1 h) for the administration of oral contrast prior to the CT scan was eliminated. Fifty-nine CT diagnoses were made of acute appendicitis, 56 of which were histologically verified and three of which resulted in another diagnosis. One hundred fourteen CT diagnoses were negative for appendicitis. This corresponds to a sensitivity of 100% and specificity of 97%, a positive predictive value of 95%, and a negative predictive value of 100%. CT with IV contrast is sensitive and specific for the confirmation or exclusion of acute appendicitis. By eliminating the time required to administer oral contrast, the diagnosis might be made more rapidly.and:Clinical guidelines, computed tomography scan, and negative appendectomies: a case series.
INTRODUCTION: Prior studies suggest that preoperative abdominal computed tomography (CT) scan can contribute to a low negative appendectomy rate. Our study objective was to evaluate cases of negative appendectomies for clinical criteria and CT use. METHODS: Retrospective 1-year study of all negative appendectomies at a community hospital. Data included clinical evidence for appendicitis as well as CT results if performed. RESULTS: Of 122 cases reviewed, 8 (6.6%) were negative appendectomies. Six were younger than 20 years. Four had a preoperative CT scan. Overall, 106 (87%) of 122 cases received preoperative CT and had a negative appendectomy rate of 3.8%. Sixteen cases did not have preoperative CT and had a negative appendectomy rate of 25% (odds ratio, 8.5; 95% confidence interval, 1.9-38.5; Fisher exact test P = .01). CONCLUSION: Patients who had a CT scan for suspected appendicitis had a lower rate of negative appendectomies than those who had no CT. Most of the negative appendectomies occurred in patients younger than 20 years.A overall negative appendectomy (NA) rate of 6.6 percent is lower than the "historically acceptable" rate of NA which is about 15 percent. The contrast between NA rates between those who received a CT and those who did not was pretty impressive. One needs to remember that the 15 percent historical rate is based on all comers. The rate will be lower in patients such as the one described above, and higher in other groups (women, extremes of age), perhaps even as low as the rates mentioned in the above studies. As a caveat I will mention that I do not have full access to the above articles. If someone else does and wishes to take issue with me, please be my guest. A third study, for which I have reviewed the entire text, is :Misdiagnosis of appendicitis and the use of diagnostic imaging.
Background
CT and ultrasound (US) are increasingly recommended to establish the diagnosis of appendicitis, but population-based rates of misdiagnosis (negative appendectomy [NA]) have not improved over time. The objective of this study was to determine the relationship between CT/US and NA in common practice.
Study design
Using data from the Group Health Cooperative on all patients undergoing appendectomy between 1980 and 1999, a longitudinal study was conducted to determine the frequency of NA over time and a case-control, medical recordÂbased study of a subset of patients from the 1990s was conducted to determine the accuracy of CT/US.
Results
Of 4,058 patients undergoing appendectomy (mean age 31 ± 18.6 [SD] years, 49.6% women), 631 (15.5%) had an NA. The overall incidence of NA remained stable over time at 1.5/10,000 patient-years, as did the age and gender adjusted rate (incident rate ratio 0.95, 95% CI 0.97, 1.01). In 1999, nearly 40% of patients had either CT or US. The aggregate sensitivity of these tests was only 74.2% (95% CI 65.7, 83.7), with a positive predictive value of 95.1% (95% CI 91.5, 96.8). CT scans were 88.3% sensitive, with 97.2% positive predictive value (95% CI 92.9, 100). Ultrasounds were 69.5% sensitive, with a positive predictive value of 94.1% (95% CI 89.6, 96.4). More than one in five tests obtained in patients with NA were positive for appendicitis (21.7% for CT and 20.8% for US).
Conclusions
The rate of NA was unchanged over time despite the introduction and use of CT/US, and this appeared to be related to the inconsistent performance characteristics of the tests. This study cautions against overreliance on CT/US in diagnosing appendicitis and emphasizes the need for test benchmarking in routine practice before establishing protocols for presumed appendicitis.
One issue I have with this study is that the most recent data is about six years old, while the data from the above studies is much more recent. CT scanning has improved much over the past six years and the techniques for performing and interpreting these studies has improved as well. Another is that from the data, the more CT/US that was done, the rate of NA fell. Looking at the following figures:
 This represents a running percentage of NA during the study period.
This represents a running percentage of NA during the study period. This represents the percentage of patients who underwent CT/US during the study period. As you can see the peak usage of CT/US correlates with reduction in the rate of NA.
This represents the percentage of patients who underwent CT/US during the study period. As you can see the peak usage of CT/US correlates with reduction in the rate of NA. And at least in my institution more than 40 percent of patients with RLQ pain are having CT/US done. Another question not answered, how many patients with "equivocal" exams were sat on and then ruptured in this study? While there is much debate on NA after CT there is little evidence that CT is missing appendicitis.
This debate will rage on, at least until studies utilizing 16 and 64 slice scanners begin to come out. For now we will have plenty to argue about. |
Thursday, December 22, 2005
Update on Dr.Roundup...
From the Atlanta Journal-Constitution:Treated patients support Stockbridge doctor.
Another shoe may be about to fall as well:
(An excellent discussion of "alternative cancer cure" testimonials by Orac may be found here)
The specifics of the charges:
My Pubmed search found this paper:Insulin-induced enhancement of antitumoral response to methotrexate in breast cancer patients
From the Atlanta Journal-Constitution:Treated patients support Stockbridge doctor.
Federal prosecutors say a Stockbridge doctor injected patients with a chemical commonly used in pesticides or weedkillers and gave desperate people false hope.
But patients like Nancy Hoffman say the hope Dr. Totada R. Shanthaveerappa instilled was real. And she wanted the world to know it. On Wednesday, the 65-year-old Stockbridge woman, dressed in a red and white pantsuit, delivered a tray of Christmas cookies to the man she says saved her life.
"This is ridiculous," she said, scowling at reporters outside his office.
Shanthaveerappa, 70, of Stone Mountain faces an 87-count federal indictment for health care fraud and money laundering involving almost $5 million. He is also known as T.R. Shantha and operates Integrated Medical Specialists, a medical clinic in Stockbridge. Federal prosecutors said he might turn himself in today.
Another shoe may be about to fall as well:
Shanthaveerappa, a native of India licensed in Georgia since 1972, is still licensed to practice medicine, but the Composite State Board of Medical Examiners has scheduled an emergency conference call Friday morning.Dr. Shanthaveerappa doesn't follow the advice of Dr. Parker:"Never be the first, or the last, to perform a procedure, or prescribe a treatment."
Dr. Jim McNatt, the board's medical director, could not say if the meeting dealt with Shanthaveerappa. The board can "issue summary suspensions if a physician is demonstrated a threat to public health and safety," McNatt said.
In a letter to a medical newsletter, Shanthaveerappa wrote that he treated a lady dying with septic shock with peritoneal hyperthermia. "The procedure has never been attempted before anywhere in the world," he wrote. "Sarcasm and indignation was expressed by my colleagues about how I treated this woman." He wrote that he is scorned by some doctors for avoiding "the status quo."Other testimonials:
Yaro Garcia and her mother, Isabell Santos, 53, came to the Stockbridge clinic from Naples, Fla., to get help for Santos' brain and breast cancer.
"Her oncologist group told us to give up, take her home and make her comfortable," Garcia said Wednesday after leaving the clinic. "But Dr. Shantha has shown us that there is no such thing as false hope. He promised to help my mom, to give her a longer life and nothing else."
[snip]
Hoffman and Denise Trinklein, who both suffer from scleroderma, a degenerative disease that affects the esophagus, agree that Shanthaveerappa is a humanitarian.
Hoffman said other doctors wanted to try traditional treatments  like steroids  but she wouldn't hear of it. "It's time people stand up to the pharmaceutical companies that are killing us," she said.
"He was doing good for mankind, more than most doctors," said Trinklein, 55, of Venice, Fla., in a telephone interview.
Trinklein said she was "desperate but informed" when she underwent a three-week intravenous chemotherapy treatment four years ago.
"People should have a choice to gamble. ... In my book of angels, he's one of them."
(An excellent discussion of "alternative cancer cure" testimonials by Orac may be found here)
The specifics of the charges:
The indictment alleges that Shanthaveerappa and medical assistant Dan U. Bartoli, 63, of McDonough defrauded health care benefit programs by falsely claiming to have performed insurance-eligible treatments by administering approved drugs. The men also allegedly used DNP, which is banned for human use in the United States.Dr. Shanthaveerappa's websites; Integrated Medical Specialists, Island of Hope (with soothing waves and music), and the wehealcancer.org site all attest to his prowess:
Think twice before you leave the U.S.A. for treatment of LYME DISEASE and CANCER or any debilitating disease such as MS, ALS, Alzheimer's, AIDS, CFS, Fibromyalgia, Gulf War Syndrome, obesity, Parkinson's, addiction, etc.He is a big fan of chelation, hyperbaric oxygen, Ukrain, and Insulin Potentiated Therapy:
Dr. Shantha has had success treating cancer, advanced cancer, stage 3 cancers, stage 4 cancers, colon cancer, breast cancer, lung cancer, liver cancer, brain cancer, prostate cancer, pancreatic cancer, ovarian cancer, mouth/throat cancer, tongue cancer, bladder cancer, small cell lung cancer, kideny[sic] cancer, bone cancer, Metastatic Cancer, Lyme Disease, Lupus, SLE, Multiple Sclerosis (MS), ALS (Lou Gherig's Disease), Sarcomas, Leukemia's, (including acute leukemia, acute lymphoblastic leukemia, acute myelogenous leukemia - AML, chronic myeloid leukemia) Melanomas, Alzheimers and other incurable illnesses.
What is IPT? IPT stands for Insulin Potentiated Therapy. In a nut-shell, by lowering ones blood sugar, cancer cells become more susceptible to any anti-cancer agents used in chemotherapy or alternative treatments. How does this work?: Cancer cells have six (6) to ten (10) times as many insulin receptor sites as healthy, well differentiated cells. This allows cancer cells to feast on sugar. By lowering your blood sugar, cancer cells open their receptors (doors) at a rate of six (6) to one (1), thereby allowing us to selectively target cancer cells while leaving healthy cells to prosper.
Therefore, lower amounts of anti-cancer agents necessary to destroy abnormal cells can be used. This improves the patients quality of life while providing the sufficient amount of therapy for reducing or ablating cancer. Side effects are significantly reduced, and your immune system doesn't take a beating.
My Pubmed search found this paper:Insulin-induced enhancement of antitumoral response to methotrexate in breast cancer patients
PURPOSE: It has been reported that insulin increases the cytotoxic effect in vitro of methotrexate by as much as 10,000-fold. The purpose of this study was to explore the clinical value of insulin as a potentiator of methotrexate. PATIENTS AND METHODS: Included in this prospective, randomized clinical trial were 30 women with metastatic breast cancer resistant to fluorouracil + Adriamycin + cyclophosphamide and also resistant to hormone therapy with measurable lesions. Three groups each of ten patients received two 21-day courses of the following treatments: insulin + methotrexate, methotrexate, and insulin, respectively. In each patient, the size of the target tumor was measured before and after treatment according to the Response Evaluation Criteria In Solid Tumors. The changes in the size of the target tumor in the three groups were compared statistically. RESULTS: Under the trial conditions, the methotrexate-treated group and the insulin-treated group responded most frequently with progressive disease. The group treated with insulin + methotrexate responded most frequently with stable disease. The median increase in tumor size was significantly lower with insulin + methotrexate than with each drug used separately. DISCUSSION: Our results confirmed in vivo the results of previous in vitro studies showing clinical evidence that insulin potentiates methotrexate under conditions where insulin alone does not promote an increase in tumor growth. Therefore, the chemotherapy antitumoral activity must have been enhanced by the biochemical events elicited in tumor cells by insulin. CONCLUSIONS: In multidrug-resistant metastatic breast cancer, methotrexate + insulin produced a significant antitumoral response that was not seen with either methotrexate or insulin used separately.Let us note the variable measured was tumor size not survival. The sites make for interesting reading and certainly prove P.T. Barnum was correct. |
(emphasis mine)
Your Papers are STILL not in Order....
Aggrivated Doc Surg warns of the danger of assimilation by JCAHO, while Ms. Schwab defends them. While I agree with the general purpose of JCAHO, a great deal of the stuff they emphasize (mission statements, QOD/QID/cc) is crap.
Posts about my last interactions with the Commission are:
Your Papers are not in Order (snarky)
Your Papers are not in Order II (examining this MSNBC report documenting the sometimes incomplete job that JCAHO does).
Remember, we (surgeons) did this to ourselves and you. Please hold your applause. |
Aggrivated Doc Surg warns of the danger of assimilation by JCAHO, while Ms. Schwab defends them. While I agree with the general purpose of JCAHO, a great deal of the stuff they emphasize (mission statements, QOD/QID/cc) is crap.
Posts about my last interactions with the Commission are:
Your Papers are not in Order (snarky)
Your Papers are not in Order II (examining this MSNBC report documenting the sometimes incomplete job that JCAHO does).
Remember, we (surgeons) did this to ourselves and you. Please hold your applause. |
Garbage In = Garbage Out....
From USA Today and the NEJM:Bad med students, bad docs:
Score another for evidence-based medicine:
If consent was obtained from these physicians, the paper fails to mention it. Why stop at medical school? Why not examine undergraduate or high school records? I blame Bush and the NSA for this.
My program director always told us that a residency program can't purge someone of their personality disorders. Goes along with the conventional wisdom of being unable to change someone after you marry them. This has been my anecdotal experience as well. In Georgia the quarterly report from the medical board has the names of physicians placed on the naughty list during that time period. Occasionally I will recognize a classmate's name and recall what a buffoon/screwball/jackass he/she was. Could have saved the board a lot of time. |
From USA Today and the NEJM:Bad med students, bad docs:
Physicians disciplined by state medical boards were three times more likely to have shown unprofessional behavior while in medical school than those with no discipline records, a study in today's New England Journal of Medicine finds.
"We found that for physicians disciplined by licensing boards, the strongest association in medical school was unprofessional behavior," says Maxine Papadakis, lead author on the study and the dean for student affairs at the University of California-San Francisco medical school.
Score another for evidence-based medicine:
Thompson, the former dean of Wake Forest University School of Medicine in Winston-Salem, N.C., says medical educators have always known intuitively that there was a connection between unprofessional behavior in medical school and later problems. But Papadakis' work "adds science at a time when we're demanding an evidence base for our judgments," Thompson says.From the abstract of the article:Disciplinary Action by Medical Boards and Prior Behavior in Medical School
Results Disciplinary action by a medical board was strongly associated with prior unprofessional behavior in medical school (odds ratio, 3.0; 95 percent confidence interval, 1.9 to 4.8), for a population attributable risk of disciplinary action of 26 percent. The types of unprofessional behavior most strongly linked with disciplinary action were severe irresponsibility (odds ratio, 8.5; 95 percent confidence interval, 1.8 to 40.1) and severely diminished capacity for self-improvement (odds ratio, 3.1; 95 percent confidence interval, 1.2 to 8.2). Disciplinary action by a medical board was also associated with low scores on the Medical College Admission Test and poor grades in the first two years of medical school (1 percent and 7 percent population attributable risk, respectively), but the association with these variables was less strong than that with unprofessional behavior.Interestingly failure of courses the first two years of school had a higher association that did failures the third or fourth years. Also academic honesty issues were not examined. How were they selected? Let us see:
The physicians who had been disciplined were graduates of three medical schools since 1970: the University of Michigan Medical School in Ann Arbor, Jefferson Medical College of Thomas Jefferson University in Philadelphia, and UCSF School of Medicine. These schools were chosen for reasons of geographic diversity and to provide representation of both public and private institutions. In addition, complete records for their graduates were available. The physicians from the University of Michigan and Jefferson Medical College included all graduates disciplined by any state medical board in the United States between 1990 and 2003. The physicians from UCSF included all graduates disciplined by any state board other than the Medical Board of California during the same period. UCSF graduates disciplined by the Medical Board of California were excluded from this study, because they had been described previously.While the disciplinary records of physicians are rightly public, aren't there some regulations about the privacy of academic records? Mind you, this isn't raw data removed of names and SSN's, these researchers had the names of disciplined physicians, and obtained their medical school transcripts. In addition, they obtained twice as many records of "non-disciplined" physicians:
All physicians were identified through a search of public records maintained in databases by the Federation of State Medical Boards. The disciplinary actions taken against physicians are available to the public according to individual state laws. The disciplinary actions range from public reprimand to revocation of the medical license. According to the Federation of State Medical Boards, even behavior that results in the least severe disciplinary action  public reprimand  may adversely affect patients. Three persons, two of whom were staff members at the Federation of State Medical Boards, classified the disciplinary actions of the state boards into three categories: unprofessional behavior, incompetence, and violation with the category not determined.
In the analysis, each physician who was disciplined was paired with two control physicians who had graduated within one year of the disciplined physician and for whom no disciplinary actions were recorded in the database of the Federation of State Medical Boards
If consent was obtained from these physicians, the paper fails to mention it. Why stop at medical school? Why not examine undergraduate or high school records? I blame Bush and the NSA for this.
My program director always told us that a residency program can't purge someone of their personality disorders. Goes along with the conventional wisdom of being unable to change someone after you marry them. This has been my anecdotal experience as well. In Georgia the quarterly report from the medical board has the names of physicians placed on the naughty list during that time period. Occasionally I will recognize a classmate's name and recall what a buffoon/screwball/jackass he/she was. Could have saved the board a lot of time. |
Wednesday, December 21, 2005
The Latest Cancer Treatment.....
Seems to involve Roundup. From MSNBC:Doctor allegedly used weed killer on patients
Dinitrophenol has been used as a weight loss aid in the past. |
Seems to involve Roundup. From MSNBC:Doctor allegedly used weed killer on patients
ATLANTA - Federal prosecutors say a doctor treated patients with cancer and other life-threatening diseases with weed killer and insecticide.
Dr. Totada Shanthaveerappa, 70, and a medical assistant face 87 counts, including health care fraud and distributing unapproved and misbranded drugs. The doctor is also charged with money laundering.
According to prosecutors, Shanthaveerappa owns and operates Integrated Medical Specialists and Integrated Chemotherapy Specialists in Stockbridge.
The clinic’s Web site says it provides “safe and effective, nontoxic, scientifically based alternative methods that can cure or control most cancer and other chronic disease.”
Prosecutors said the doctor and assistant Dan Bartoli, 63, injected numerous patients with unapproved and misbranded drugs, including Dinithrophenol, a commercial-grade weed killer and insecticide.
The two men also submitted false insurance claims which disguised the types of drugs and treatments they were providing, according to the indictment.
Prosecutors did not claim that anyone suffered any direct harm from the treatments.
Shanthaveerappa and Bartoli did not immediately return telephone calls Tuesday night.
Dinitrophenol has been used as a weight loss aid in the past. |
Tuesday, December 20, 2005
Grand Rounds Vol II, No. 13
Dr. Smith at Medpundit hosts Grand Rounds this week. A wonderful effort by the Grand Dame of the medical blogosphere. |
Dr. Smith at Medpundit hosts Grand Rounds this week. A wonderful effort by the Grand Dame of the medical blogosphere. |
Monday, December 19, 2005
Tales from the Trauma Service XIII.....
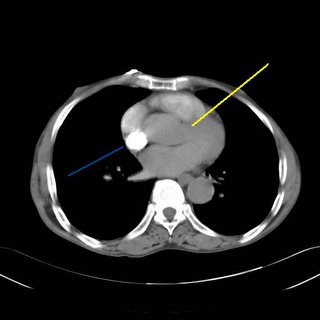
Every once in awhile you come across a radiographic finding that looks "just like in the book".
Young man falls from a second story window. Arrives somnolent but will awaken to voice. Multiple episodes of nausea and vomiting.
The images:

Small parenchymal bleed.
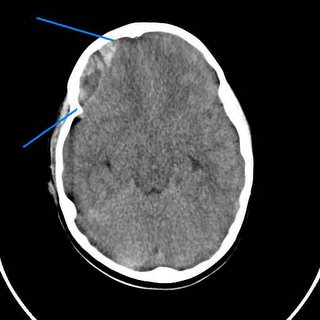
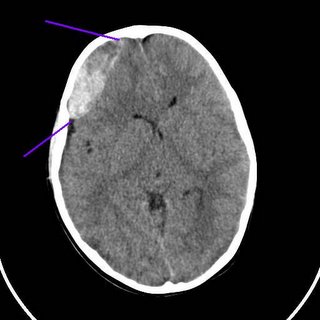
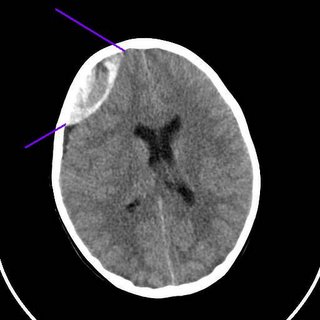
The classic radiographic appearance of an epidural hematoma. The neurosurgeon took him to the operating room for a decompressive craniotomy.
Every once in awhile you come across a radiographic finding that looks "just like in the book".
Young man falls from a second story window. Arrives somnolent but will awaken to voice. Multiple episodes of nausea and vomiting.
The images:

Small parenchymal bleed.
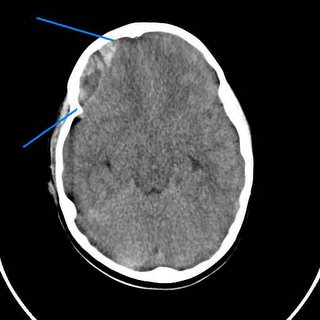
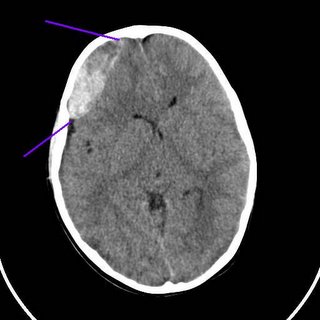
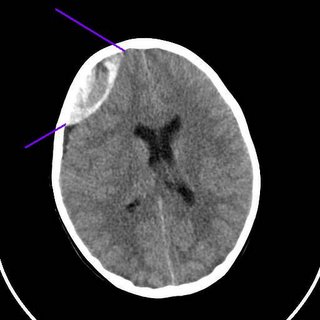
The classic radiographic appearance of an epidural hematoma. The neurosurgeon took him to the operating room for a decompressive craniotomy.
Labels: Tales from the Trauma Service
|Thursday, December 15, 2005
What does the Red State Moron Think of this??
Cosmetic surgery "below the equator", via the Wall Street Journal:Virgin Territory: U.S. Women Seek A Second First Time
So Dr. Wigton, something to think about if you give up high-risk OB. |
Cosmetic surgery "below the equator", via the Wall Street Journal:Virgin Territory: U.S. Women Seek A Second First Time
For her 17th wedding anniversary, Jeanette Yarborough wanted to do something special for her husband. In addition to planning a hotel getaway for the weekend, Ms. Yarborough paid a surgeon $5,000 to reattach her hymen, making her appear to be a virgin again.Beats a pair of socks, I guess. This procedure has led to some unusual promotions:
"It's the ultimate gift for the man who has everything," says Ms. Yarborough, 40 years old, a medical assistant from San Antonio
"Revirgination" costs as little as $1,800 at Ridgewood Health and Beauty Center, a spa and cosmetic-surgery center in the New York City borough of Queens. To promote the procedure, the center's owner, Cuban-born Esmeralda Vanegas, has given away hymenoplasties on a Spanish-language radio station. She also promotes them in her eponymous magazine, Esmeralda.Some have procedures performed to improve their sex lives:
Dr. Pelosi says an increasing number of patients are trying to "improve their sex lives" by combining hymen repair with an operation to tighten their vaginas. He says one patient did it to surprise her husband on a second-honeymoon cruise. Another patient, a 51-year-old Manhattan attorney and mother of three, had him reattach her hymen and tighten her vaginal walls in 2003. "I thought it would add that extra sparkle to our marriage," says the woman.Hymenoplasty carries little risk, except prehaps to one's wallet:
The modern version of hymenoplasty requires a local anesthetic and no hospitalization. A doctor uses dissolvable stitches to reconnect the skin membrane that once partially covered the opening to the vagina. Intercourse will tear the membrane causing pain and bleeding.With insurance reimbursement drying up, gynecologists are expanding their "cash only" trade.
Recovery from surgery takes about six weeks. The risk of fever and infection is low, says V. Leroy Young, a St. Louis plastic surgeon who also heads the American Society of Plastic Surgeons' emerging-trends task force.
On the other hand, Dr. Young says, "it's a pretty expensive thing to do for one night."
Troy Robbin Hailparn, an obstetrician and gynecologist, advertises vaginal cosmetic surgery on 23 billboards around San Antonio. Edward Jacobson, a Greenwich, Conn., OB-GYN, offers vaginal-makeover packages for international patients that include airfare, limousine travel and hotel accommodation. Dr. Jacobson says he has advertised in Glamour, Harper's Bazaar and Allure magazines. Last year, David Matlock, an OB-GYN in Los Angeles, discussed his "Laser Vaginal Rejuvenation" practice on "Dr. 90210," a reality show on the E! cable network.Who's not happy? The OB/GYN establishment:
The ethics committee of the American College of Obstetricians and Gynecologists, concerned about the marketing of revirgination, sent a letter to several cosmetic gynecologists in June 2004 voicing its unease. The college, which hasn't taken a formal position on the matter, said it worried that doctors may not be able to fully inform their patients about the procedure because it doesn't appear in the medical literature."Feminists":
Thomas G. Stovall, a recent president of the Society of Gynecologic Surgeons, a top professional body, says "hymen repair is a totally bogus procedure." In general, he says, surgery marketed to improve one's sex life rarely works. As for hymen replacement, "most importantly, it doesn't make you a virgin again."
A 26-year-old Latin American woman who lives in New York's Queens had a hymen repair in 2001 and says it took almost two months for her to feel comfortable again. It took even longer for her to enjoy sex.And religious folk:
The married mother of two says she's glad she had the surgery nonetheless. She says her husband wanted to experience intercourse with a virgin. "If a woman isn't a virgin when she gets married, a man can always put her down for that," says the woman, who does part-time clerical work for Ms. Vanegas's Ridgewood clinic.
Such attitudes irk feminists, who say hymen repair is a manifestation of bigger social pressures that keep women subservient to men. "It comes with a whole set of norms of a macho culture," says Silvana Paternostro, Colombian-born author of "In the Land of God and Man: Confronting Our Sexual Culture."
Devout Roman Catholics prize virginity because sex before marriage is a sin. Hymen replacement is "misleading and misguided," says Kathleen Raviele, vice president of the Catholic Medical Association in Needham, Mass., and a gynecologist. "The best thing is to remain chaste until marriage and then have that genuine experience on your wedding night."Whatever floats your boat, I guess. I agree with Dr. Young's opinion about it being an awfully expensive "one night stand".
For many Muslims, sexual purity is a way of maintaining the sanctity of the family. But Islamic law also prohibits lying and frivolous cosmetic surgery, says Uzma Mazhar, a St. Louis psychotherapist known for her Web site, CrescentLife.com, which provides Islamic perspectives on Western issues.
"What people forget is that Islam teaches us to be honest and fair," Ms. Mazhar says. "A family should think about this before they present a woman as a virgin when she's not."
So Dr. Wigton, something to think about if you give up high-risk OB. |
Tuesday, December 13, 2005
Grand Rounds Vol 2 No. 12....
Dr. Lowe hosts Grand Rounds from the part of Big Pharma that doesn't roll around naked in rooms full of money. |
Dr. Lowe hosts Grand Rounds from the part of Big Pharma that doesn't roll around naked in rooms full of money. |
Monday, December 12, 2005
Cool CT Stuff....
50-ish male with diagnosis of colon cancer about 2 years ago. He declined treatment at that time so he could "go off and drink". He returns now with severe anemia with a hemoglobin of 4.5. He is now amenable to surgery. A CT was obtained to evaluate his liver:


Chock-full o'mets, as expected. But an interesting finding more superiorly:
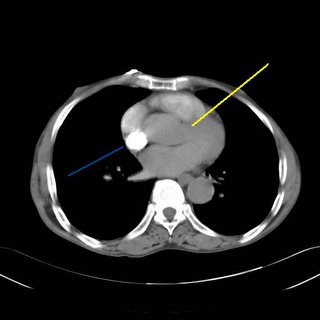

Contrast fills the right heart (blue) but does not fill the left side (yellow). Whatever is wrong? Could it be a mistimed contrast injection? Not according to the radiologist. An asymptomatic PE, it appears, is what we have:


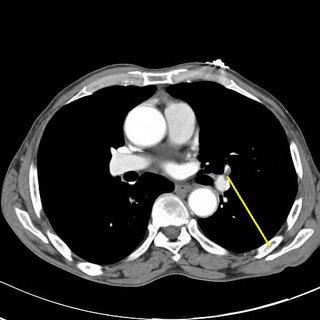
Clot marked in yellow.
Pretty cool, huh? |
50-ish male with diagnosis of colon cancer about 2 years ago. He declined treatment at that time so he could "go off and drink". He returns now with severe anemia with a hemoglobin of 4.5. He is now amenable to surgery. A CT was obtained to evaluate his liver:


Chock-full o'mets, as expected. But an interesting finding more superiorly:

Contrast fills the right heart (blue) but does not fill the left side (yellow). Whatever is wrong? Could it be a mistimed contrast injection? Not according to the radiologist. An asymptomatic PE, it appears, is what we have:


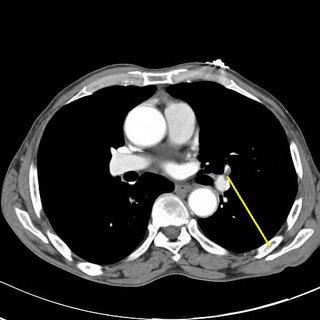
Clot marked in yellow.
Pretty cool, huh? |
Thursday, December 08, 2005
Healthcare in the Worker's Paradise....
Think the uninsured have it tough here? How about the People's Republic of China? From The Wall Street Journal:Chinese Doctors Tell Patients To Pay Upfront, or No Treatment
The physicians seem to be a bunch of heartless bastards:
Think the uninsured have it tough here? How about the People's Republic of China? From The Wall Street Journal:Chinese Doctors Tell Patients To Pay Upfront, or No Treatment
As soon as the money dries up, doctors warn, so will the drugs that could save the life of Cui Guangshun's 7-year-old son, Dejie, in the leukemia unit of Beijing Children's Hospital.No such thing as EMTALA in China:
Such are the rules of China's pay-as-you-go health system: cash upfront, or no treatment.
Mr. Cui's wife, Yang Deyin, traveled more than 300 miles by bus to Beijing from their small farm on the grasslands of Inner Mongolia to be near her only child. For weeks, she camped out on a blue plastic chair in one of the hospital waiting rooms to save money on lodging, like dozens of other parents.
Back home, her husband pleaded with relatives and village neighbors for more loans to keep the boy's care going. Most nights, the mother queued up in a drab hospital lobby, littered with food wrappings and possessions, to use a touch-screen computer that told her how much of the family's cash was left. Sometimes the number flashed red, meaning the family was in arrears and prompting a frantic call to her husband.
In the past few weeks, Mr. Cui and Ms. Yang have been forced to accept a terrible reality: Even though their son's leukemia is considered highly treatable, they may never raise enough money to cure him. The hospital's estimated fees of $18,500 to complete an initial 6½-month course of treatment are impossibly high set against the family's annual income of less than $350. Like two-thirds of China's population, they don't have health insurance.
"There's nothing for it," Mr. Cui sighed, slumped in the doorway of his red brick home on a recent afternoon. He said he had dug up his potato crop and sold it all. He had threshed his corn and sold most of that, too, leaving barely enough to make the steamed bread that keeps his family going through the winter. "I'll just have to fetch Dejie home to die," he said.
A year ago, Sam Lin, a prosperous factory owner, took his pregnant wife to a hospital in the southern boomtown of Shantou to give birth. As he recalls it, the couple were startled in the waiting room of the maternity wing by a commotion. A woman who had just delivered her baby was bleeding profusely and needed an emergency blood transfusion. Mr. Lin heard nurses screaming at the bleeding woman's husband. "If you don't have any money, we don't operate," one yelled, according to Mr. Lin. He says he rushed up to the man, counted out a stack of banknotes and thrust them on him. He never found out whether his charity saved the woman's life.These physicians seen to engage in "defensive medicine for fun and profit":
Today, China has plenty of large hospitals packed with state-of-the-art equipment to compete for paying patients. To maximize revenue, hospital doctors routinely overprescribe drugs and diagnostic procedures, according to studies by the Chinese government and international bodies like the World Bank. Hospitals sell many drugs directly to patients and add a profit margin.
A World Bank study estimates that drugs account for more than 50% of all Chinese health spending. In the U.S., prescription drugs account for less than 15% of total health spending, according to U.S. government figures. The World Bank study says 12% to 37% of Chinese national health expenditures are wasted because of unnecessary drug prescriptions.
"Hospitals have become huge corporate profit centers," says Chen Bowen, an official with the Society of Community Health Service, a nonprofit organization based in Beijing that advises authorities on health reform.
The physicians seem to be a bunch of heartless bastards:
At the Beijing Children's Hospital, doctors in the cancer ward quickly got to the bottom line. They explained to Dejie's mother that if the family's account dipped into arrears, that would be the end of the boy's treatment.There's more:
The hospital's Dr. Xie says doctors' income would be affected if they don't "push patients hard enough" to settle their bills. "Nowadays, doctors don't just treat patients. They've also got to chase for payment," she says.
According to hospital regulations, once patients owe more than $250, the doctor must issue a warning and take responsibility for getting the money. Usually patients pay in cash. Credit cards aren't widely used in China. "Hospitals are not charities," says Dr. Xie. "The biggest problem is the poor insurance system.".....
......The next day, Mr. Cui made the long road trip to Beijing and stood meekly by his wife as one of the doctors scolded them for getting behind on their payments. "We warned you about this at the very beginning," the doctor said, barely glancing up as her fingers tapped out a message on her mobile phone. "Now you've lost all your money and you'll lose the boy too." Mr. Cui stared down at his feet. His wife said nothing, but her eyes filled with tears.
Medical horror stories have become a staple of Chinese state newspapers and investigative television shows. Last month, the China Youth Daily reported that the impoverished family of a 47-year-old migrant worker left her for dead at a crematorium in the eastern city of Taizhou after checking her out of a hospital where she was admitted with a brain hemorrhage. The woman was saved after undertakers noticed her hand moving and saw tears in her eyes. A hospital official confirmed the details of the story, and said the woman was now back in the hospital after donations poured in. The family apparently left her because they were too poor to pay for the treatment.Government programs aside, demographics are working against the Chinese. With the "one child" policy in effect for so long the mean age of the population is rising, and there may not be enough workers to financially support the elderly in the coming years. |
Tuesday, December 06, 2005
Monday, December 05, 2005
Skill Versus Judgment.....
In a comment to this post my neurologist colleague Greg P. posted:
But would the training be complete? Hardly, in my opinion. But those on the other side of the "surgeon as technician" debate, would differ.
"Surgical judgment", on the other hand, is something that has to be learned, for the most part. I say "for the most part" because the foundation for surgical judgment comes from the knowledge one accumulates from reading textbooks or sitting in lectures. This is the "don't cut the common bile duct or bad things will happen" type stuff that you pick up along the way. This, along with experience, molds one's surgical judgment over time. It forms a feedback loop of sorts, as this Quotation From Training demonstrates:
Now there are some surgeons out there that can acquire skill and judgment more quickly and less painfully than others. Surgery has its' "naturals" like every other profession. Most are "skills" naturals rather than "judgment" naturals.
As for me, while I would like my surgeon to have both good skills and judgment, I would pick the one with good judgment/mediocre skills over one with mediocre judgment/good-great skills because the surgeon with superior judgment recognizes their limitations and will adjust while the "technical wizard" can find themselves in trouble very easily. |
In a comment to this post my neurologist colleague Greg P. posted:
One of my colleagues (also not a surgeon) suggested once that the diagnostic and judgment skills and the technical operating skills of surgeons can many times be independent features of a surgeon. One would always hope that ones own surgeon is good at both, but one can certainly sense that some surgeons are much better at one than the other.In my opinion, technical skills and judgment are developed separately. Since while one of those qualities can be taught, the other must be learned. The difference being is that the technical aspects of an operation can be learned from a book or other means. The time may come in the near future when a surgical resident can learn and practice a procedure on a simulator multiple times prior to performing it on a live patient. This would allow for the ultimate refinement of technique in an atmosphere of no risk to a live patient.
But would the training be complete? Hardly, in my opinion. But those on the other side of the "surgeon as technician" debate, would differ.
"Surgical judgment", on the other hand, is something that has to be learned, for the most part. I say "for the most part" because the foundation for surgical judgment comes from the knowledge one accumulates from reading textbooks or sitting in lectures. This is the "don't cut the common bile duct or bad things will happen" type stuff that you pick up along the way. This, along with experience, molds one's surgical judgment over time. It forms a feedback loop of sorts, as this Quotation From Training demonstrates:
"Good judgment comes from experience, experience comes from bad judgment"So you have to learn (sometimes painfully) judgment. You learn from your mistakes. Some good examples of this come from a show that I initially had little nice to say about but I have grown to appreciate: Grey's Anatomy. Dr. Alex Karev gives a patient too much hypertonic saline and it causes complications. At the end, Dr. Shepherd speaks to him about "the first patient I killed". That experience left an indelible mark on him. That's not something that can be taught. Same thing for Izzie's "distance problem" I have said it before operating is easy, surgery is hard.
Now there are some surgeons out there that can acquire skill and judgment more quickly and less painfully than others. Surgery has its' "naturals" like every other profession. Most are "skills" naturals rather than "judgment" naturals.
As for me, while I would like my surgeon to have both good skills and judgment, I would pick the one with good judgment/mediocre skills over one with mediocre judgment/good-great skills because the surgeon with superior judgment recognizes their limitations and will adjust while the "technical wizard" can find themselves in trouble very easily. |
Sunday, December 04, 2005
From The Onion:
"C-Sections On The Rise"
My favorite:
"C-Sections On The Rise"
My favorite:
"These things are being overperformed. I went in for an appendectomy and came out with a healthy baby boy."|
Saturday, December 03, 2005

Georgia 34 LSU 14

University of Georgia: 2005 Southeastern Conference Champions.
Next stop: The Sugar Bowl against the West Virginia Mountaineers. |





