Sunday, January 30, 2005
Saturday, January 29, 2005
Bad Weather....
Ice storm makes it's way through the southeast. Lots of people living near Dr. Parker lost power, but fortunatley we did not. Pictures of the back forty:


 |
|
Ice storm makes it's way through the southeast. Lots of people living near Dr. Parker lost power, but fortunatley we did not. Pictures of the back forty:


 |
|
Mismatch Problem....
Mr. Genes reports on a fourth-year student's worse nightmare. What if the match is screwed up? That is what happened with the AUA's Urology match this year. There was a problem with the computer and several top programs were unfilled. The match was rerun and the discussion board that Mr. Genes links to has future urologists giving their "false" results and "true" results. My heart goes out to those that had matched at first, but did not match during the "second" match. Many cancelled other interviews and others had program directors berate them.
Hopefully the good people at the NRMP are paying attention. |
Mr. Genes reports on a fourth-year student's worse nightmare. What if the match is screwed up? That is what happened with the AUA's Urology match this year. There was a problem with the computer and several top programs were unfilled. The match was rerun and the discussion board that Mr. Genes links to has future urologists giving their "false" results and "true" results. My heart goes out to those that had matched at first, but did not match during the "second" match. Many cancelled other interviews and others had program directors berate them.
Hopefully the good people at the NRMP are paying attention. |
Thursday, January 27, 2005
Georgia Tort Reform Update....
From the Athens Banner-Herald:New committee named to examine tort reform
The hope is that by streamlining the process the likelihood of passage will increase. We shall see.
The first bill, Senate Bill 3 is in committee this week. I'm keeping my fingers crossed. |
From the Athens Banner-Herald:New committee named to examine tort reform
House Speaker Glenn Richardson was expected today to name Harlem Republican Rep. Barry Fleming as chairman of a special committee to handle the combustible issue of tort reform.
Fleming said the committee, to be called the Special Committee on Civil Justice Reform, would likely meet in the next couple of weeks to begin handling the controversial question of restrictions on medical-malpractice lawsuits.
The hope is that by streamlining the process the likelihood of passage will increase. We shall see.
The first bill, Senate Bill 3 is in committee this week. I'm keeping my fingers crossed. |
Tuesday, January 25, 2005
Grand Rounds XVIII

Hospital Amphitheater Clinic (1927)
Early in the morning before the sun is up, the pre-rounds have already been done and the disturbed patients have returned to their slumber. No drug-rep money for this conference so the breakfast fare is the standard plastic cups of juice, bad coffee, and Sam's Club danish. The auditorium fills up with attendings, residents, and students. Their place on the hierarchy can be determined by their state of dress, (unless there are resident interviewees present and they will be the best dressed of all). At the appointed hour the presenter arises to the podium and Grand Rounds, surgical style, kicks off:
Dr. Charles treats a patient that conjures up a home remedy. He then counters with his own potion:
The Medical Madman writes about what could happen if Scrubs met The Stepford Wives:Perfect-Resident Life:
Kevin MD shares the story of a patient with swollen shoulders:
Medviews wonders if the advent of Medical Savings accounts will lead to hucksterism:
How about free toasters? I could give out Ginsu knives!!!
Saint Nate offers up a great moment in socialized medicine.
A glimpse of the future?
Shrinkette offers up a link-filled tribute to nursing colleagues:
One of those angels is Geena of Codeblog who falls into the tender trap of making it personal:
Another nurse at The Write Wing relates how the simplest thing can bring back a memory:
My comrade-in-arms Orac shares his thoughts on the fact that denial is more that a river in Egypt, and sometimes the most obvious question is maybe not appropriate:
Hey you in the back!!! Wake up!!!
The Cheerful Oncologist reminds us that healing is more than cutting out disease or repair of injury:
Matthew Holt dissects the shutdown of King-Drew Medical Center in Los Angeles (which included a busy trauma center). An excellent discussion of a community's antagonistic relationship with "the man" as well as the hospital as political machine:
Speaking of putting it to "the man" Mr. McBride embarks on a one-man crusade to shift thinking within the AMA:
Dr. Centor takes another look at the problem of "cherry picking":
A bottle in front of me or a frontal lobotomy? Dr. Emer reports, you decide:
Speaking of happy hour: The Hospice Blog raises a glass to the availability of generic Duragesic patches:
Schools screen for hearing, vision, scoliosis and lead exposure. Dr. Baker explains why screening for mental illness may raise objections:
The Journal Club takes issue with the NEJM report comparing aspirin versus Plavix:
I don't submit "show-and-tell" posts since many of the photographs I post aren't suitable for work. This week's photo essays are
Doctor Bob's review of kidney stone treatment and the Grunt Doc's review of his antibacterial hand cleaner. Safe for work? Depends on the imagination of your co-workers.
The weekly lecture over, the masses in various states of somnolence, cleanliness, and attentiveness shuffle out of the room. Some to round, some to the OR and a lucky few to home, family, and a warm bed. Until next week.
Thanks to all who submitted posts. Grand Rounds XIX will be hosted next week by Ms. Pelletier at Daily Capsules. Grand Rounds are archived at an Undisclosed Location. A special thanks to Mr. Genes at Blogborygmi for starting the ball rolling. |

Hospital Amphitheater Clinic (1927)
Early in the morning before the sun is up, the pre-rounds have already been done and the disturbed patients have returned to their slumber. No drug-rep money for this conference so the breakfast fare is the standard plastic cups of juice, bad coffee, and Sam's Club danish. The auditorium fills up with attendings, residents, and students. Their place on the hierarchy can be determined by their state of dress, (unless there are resident interviewees present and they will be the best dressed of all). At the appointed hour the presenter arises to the podium and Grand Rounds, surgical style, kicks off:
Dr. Charles treats a patient that conjures up a home remedy. He then counters with his own potion:
It was important that I leave the room as soon as possible, before the exchange of sorcery escalated any further. We had matched wits and I was satisfied that I had withstood her.Calling Doctor Bombay !!! Calling Doctor Bombay !!!
The Medical Madman writes about what could happen if Scrubs met The Stepford Wives:Perfect-Resident Life:
I predict a revolution. By mid-summer, with a new model up and running, Perfect-Resident will be a reality, a reality which will shake Graduate Medical Training at its core. Get ready for the new improved prototype of graduate whose soul purpose in life will be to admit, obey and do as little thinking as possibleConsider the 80 hour problem solved.
Kevin MD shares the story of a patient with swollen shoulders:
A 66-year-old man presented with a two-year history of fatigue, paresthesia of the legs and feet, weight loss, and shoulder enlargement, with limitation of movement.The diagnosis is not what you would think from looking at the photograph.
Medviews wonders if the advent of Medical Savings accounts will lead to hucksterism:
How will primary care providers behave if health savings accounts take hold? Some may advertise their services in the media, as in "I will give you a physical exam for $200, and I'll throw in a free nutritional evaluation for the first 100 cust..., I mean patients."
How about free toasters? I could give out Ginsu knives!!!
Saint Nate offers up a great moment in socialized medicine.
Also, what's with her needing a doctor's referral for an emergency where every minute counts? And then telling her to go to a different hospital ... I don't know how Mr. Wright took it so well, I'd be banging on whatever--paperpusher-told-me-that's desk demanding she be admitted.
A glimpse of the future?
Shrinkette offers up a link-filled tribute to nursing colleagues:
As a nurse you sacrifice a little of yourself: your time, your energy, your dignity, your lunch, your need to pee. But the end result, your impact on your patients and their lives, makes the job worth while.
The end result helps me get up the next morning, report to the unit at seven o' clock, and do it all over again.
One of those angels is Geena of Codeblog who falls into the tender trap of making it personal:
I have lost objectivity with this patient....... I am giving the patient the best nursing care that I know to give, but still the nagging in the back of my mind continues... I am not doing everything to help alleviate this patient's suffering. But who am I to make such a decision? They teach us about being a patient advocate in nursing school, to do what's in the patient's best interest. And I want to do that. Every single doctor and nurse on this case knows how this will end. Does this sound harsh to the lay-person or medical professional who is not intimately aware of the realities of ICU?Sometimes we do treat the family rather than the patient.
Another nurse at The Write Wing relates how the simplest thing can bring back a memory:
When I left for the night, I stopped for a cigarette at the spot by the garden where I had found Jimmy. Some of the flowers were splattered with his blood.
I don't think I had thought about him until the other day when I picked up my child at school and a boy yelled "Jimmy!" -- that was all it took. I could see the flowers, and his blond hair. I took a deep breath, and went on with life.
My comrade-in-arms Orac shares his thoughts on the fact that denial is more that a river in Egypt, and sometimes the most obvious question is maybe not appropriate:
This patient was in her early 60's, most definitely not poor, and with a close family. She presented not just with a large tumor, but with a large, nasty, fungating, bleeding tumor that was eroding through the skin of her breast. It was a real problem, not just because it was a locally advanced cancer, but because it was intermittently bleeding a lot. Even worse, it smelled. Part of the tumor had become necrotic (dead) and was rotting....As a junior resident, unexperienced in these matters, at one point I asked her a very stupid question: "What did you think was going on here?"His experience has taught him that the question can be best asked later.
Hey you in the back!!! Wake up!!!
The Cheerful Oncologist reminds us that healing is more than cutting out disease or repair of injury:
Healing is more than just a purging of illness...it is peace of mind, which provides a greater benefit than the doctor's potions. Peace of mind is the elixir of renewal, which lifts the sun up over the horizon in the morning, showing the world that we are ready to meet the day's challenges. It is the healing that once applied, never dies.So physician, heal thyself.
Matthew Holt dissects the shutdown of King-Drew Medical Center in Los Angeles (which included a busy trauma center). An excellent discussion of a community's antagonistic relationship with "the man" as well as the hospital as political machine:
Finally, whenever you have a huge public health system like that of New York or Los Angeles, you are going to inevitably have to deal with the politicization of running it. Just understanding the bureaucracy of hiring and firing in these huge government departments boggles the mind of those of us used to the private sector. The delivery of favors and appointments in returns for influence, votes, and union members' electoral work continues to be standard practice in most city governments in the US (and has its direct equivalent at a national level!).A problem not confined only to big cities.
Speaking of putting it to "the man" Mr. McBride embarks on a one-man crusade to shift thinking within the AMA:
So there you have it folks! You have to first join an organization with immoral policies that go against the ethics of the profession before having a prayer of changing said policies. And then, you only get one vote out of roughly a million. And you would be voting against people who are voting in self-interest. HmmmDo you light a candle or rage against the darkness?
Dr. Centor takes another look at the problem of "cherry picking":
The idea behind report cards seems sound, but what are the unintended consequences. Is the public health better, or do we have cardiologists "cherry picking" healthier patients and eschewing the more complex? Perhaps the report cards create a Catch-22 for some patients!Which is worse, a sin of commission or a sin of omission?
A bottle in front of me or a frontal lobotomy? Dr. Emer reports, you decide:
Women who consistently were drinking about ½ to 1 drink per day had both less cognitive impairment as well as less decline in their cognitive function compared to women who didn't drink at all," Grodstein said.Bottle of wine, fruit of the vine.....
Speaking of happy hour: The Hospice Blog raises a glass to the availability of generic Duragesic patches:
Off the top of my head Id say that over 50% of our patients use the patches at some point while on service. Few use as much as the example above, but if a hospice has 20 patients on patches their savings could be up to $2,000 a month. You can dang near hire another full time nurse for that!
Schools screen for hearing, vision, scoliosis and lead exposure. Dr. Baker explains why screening for mental illness may raise objections:
Why does the New Freedom Commission rec stir up such a fuss? One word answer: stigma.Does this make ADHD a "stigma"?
In the words of one who lives with a mental disorder: "people don't feel like they've failed if they have asthma or diabetes, why should those of us who suffer from mental illness feel that, somehow, all we are is "crazy?"
The Journal Club takes issue with the NEJM report comparing aspirin versus Plavix:
This is a very unsatisfying comparison. On the one hand a drug, aspirin, that is clearly ulcerogenic and also promotes bleeding taken together with a drug that effectively prevents ulcers (omeprazole). On the other hand, a drug (Plavix) that may be less ulcerogenic but is even more likely to promote bleeding and given without any ulcer prevention. This comparison just muddies the waters. This study does not help distinguish the platelet-antagonizing effect of clopidogrel from any direct effect on the healing or ulcers.The Rebel Doctor also weighs in. My use of Plavix is reserved for patients with new endovascular stents.
I don't submit "show-and-tell" posts since many of the photographs I post aren't suitable for work. This week's photo essays are
Doctor Bob's review of kidney stone treatment and the Grunt Doc's review of his antibacterial hand cleaner. Safe for work? Depends on the imagination of your co-workers.
The weekly lecture over, the masses in various states of somnolence, cleanliness, and attentiveness shuffle out of the room. Some to round, some to the OR and a lucky few to home, family, and a warm bed. Until next week.
Thanks to all who submitted posts. Grand Rounds XIX will be hosted next week by Ms. Pelletier at Daily Capsules. Grand Rounds are archived at an Undisclosed Location. A special thanks to Mr. Genes at Blogborygmi for starting the ball rolling. |
Monday, January 24, 2005
Final Call for Submissions....
Important events and people are often associated with Roman numerals: monarchs and popes, space flight, world wars, Super Bowls,and....Grand Rounds!!
Send in your submission for Grand Rounds XVIII by 9PM EST today. Either leave permalink in the comments section or email them to me :cut_to_cure-at-hotmail.com.
Thanks for your support!! |
Important events and people are often associated with Roman numerals: monarchs and popes, space flight, world wars, Super Bowls,and....Grand Rounds!!
Send in your submission for Grand Rounds XVIII by 9PM EST today. Either leave permalink in the comments section or email them to me :cut_to_cure-at-hotmail.com.
Thanks for your support!! |
Sunday, January 23, 2005
Call for Submissions.....
The eighteenth edition of Grand Rounds, the weekly exposition of the medical blogosphere's best will be held here on Tuesday, January 25, 2005.
Submissions may be sent either by email : cut_to_cure-at-hotmail.com, or left in the comments section below.
Submission deadline is 9:00 PM EST on Monday, January 24, 2005.
Happy posting.
Want to host Grand Rounds in the future? Contact Mr. Genes over at Blogborygmi. |
The eighteenth edition of Grand Rounds, the weekly exposition of the medical blogosphere's best will be held here on Tuesday, January 25, 2005.
Submissions may be sent either by email : cut_to_cure-at-hotmail.com, or left in the comments section below.
Submission deadline is 9:00 PM EST on Monday, January 24, 2005.
Happy posting.
Want to host Grand Rounds in the future? Contact Mr. Genes over at Blogborygmi. |
Your Midlife Crisis could Kill You....
From the Atlanta Journal-Constitution, among others, Motorcycle fatality trends worry officials:
The older crowd also is more likely than younger motorcyclists to ride while intoxicated and to ride without a helmet.
So you might want to stick with the hair transplants or the Porsche and avoid the Harley. |
From the Atlanta Journal-Constitution, among others, Motorcycle fatality trends worry officials:
Mike Cullinan made a midlife course correction, breaking up with his girlfriend and buying a Harley-Davidson motorcycle: a 620-pound Dyna Low Rider with a 1,450-cc, fuel-injected engine.In going against the usual trend in trauma, the victims are getting older:
Lots of baby boomers and middle-age Americans like Cullinan, 38, are getting motorcycles, whether to recapture their lost youth or pull through some kind of midlife crisis.
As a result, riders 40 and over are accounting for an alarming number of motorcycle deaths.
Safety experts suspect that older riders with a lot of disposable income are buying more machine than their out-of-practice bodies can handle.
Across the country, the annual number of motorcycle fatalities among 40-plus riders tripled in the past decade to 1,674 in 2003, while deaths among riders under 30 dropped slightly to 1,161, according to the National Highway Traffic Safety Administration.
According to the NHTSA, the average age of motorcyclists killed in accidents rose from 32 in 1994 to 38 in 2003.Older drivers are buying larger and more powerful motorcycles and their abilities aren't what they used to be:
''It's really kind of astonishing. The ages of these fatalities are so high. You would think it would be all of the young kids on those fast bikes, but it's not,'' said Carl Hallman, highway safety coordinator with the Maine Department of Public Safety.
The surge in deaths among older riders helped push motorcycle fatalities higher overall. They jumped by nearly half during the past five years, from 2,483 in 1999 to 3,661 in 2003.
''They haven't ridden in 20 or 30 years, so their skills are rusty. Motorcycles have changed, and they're getting bigger motorcycles. And they're getting on without a refresher course,'' said Cathy Rimm, program director for Motorcycle Rider Education of Maine, a nonprofit organization that offers safety training.
The older crowd also is more likely than younger motorcyclists to ride while intoxicated and to ride without a helmet.
So you might want to stick with the hair transplants or the Porsche and avoid the Harley. |
Thursday, January 20, 2005
If you Don't Break Ribs you Aren't Doing it Right...
At least that is what I was told when taking BLS and ACLS. According to The New York Times some don't like the snap, crackle, and pop:
CPR Is Often Done Wrong, Studies Find:
So I guess we need to push harder. |
At least that is what I was told when taking BLS and ACLS. According to The New York Times some don't like the snap, crackle, and pop:
CPR Is Often Done Wrong, Studies Find:
Cardiopulmonary resuscitation is often inadequately performed by doctors, paramedics and nurses, two studies of resuscitation efforts during cardiac arrest have found.
Two common problems are rescuers not pushing hard enough or frequently enough on the chest to restart the heart, and rescuers breathing air into the lungs too often, either mouth to mouth or through tubes.
In a study that involved 67 adults at the University of Chicago, doctors and nurses failed to follow at least one CPR guideline 80 percent of the time. Failure to follow several guidelines was common.
The other study involved 176 adults with out-of-hospital cardiac arrest treated by paramedics and nurse anesthetists in Akershus, Norway; London; and Stockholm. Chest compressions were done half the time, and most were too shallow.
Both studies used an experimental monitor that assesses CPR quality, and both received financing from Laerdal Medical, a Norwegian company that developed the monitor with Philips Medical Systems, a subsidiary of Royal Philips Electronics of Amsterdam.
The studies appear in The Journal of the American Medical Association.
So I guess we need to push harder. |
Tuesday, January 18, 2005
The Future of Medical Specialists....
A hat tip to Kevin for this American Medical News link:Cardiologists pump up efforts to avert shortage. I can remember a time when the words "shortage of" and "cardiologists" were not used in the same sentence unless linked with the words "jobs for". How times change.
One controversial proposal would involve the creation of a cardiology track which would eliminate the third year of an internal medicine residency. Before all you wannabe cath jockeys get excited, look at the details:
Just wait, soon an internal medicine career path can look like this one:
 |
|
A hat tip to Kevin for this American Medical News link:Cardiologists pump up efforts to avert shortage. I can remember a time when the words "shortage of" and "cardiologists" were not used in the same sentence unless linked with the words "jobs for". How times change.
One controversial proposal would involve the creation of a cardiology track which would eliminate the third year of an internal medicine residency. Before all you wannabe cath jockeys get excited, look at the details:
Residents in cardiology programs now spend three years in internal medicine, followed by three years in cardiology. They then can opt for an additional year in a subspecialty.Ah yes, five years for a non-invasive cardiologist. I don't know if they would still learn how to perform diagnostic caths or not. What would the "five-year wonder" get?
The ACC would like to add an alternative five-year program that eliminates the third year of internal medicine and cuts out training in the high-tech cardiology procedures.
Steve Fihn, MD, MPH, a past president of the Society of General Internal Medicine and a professor of medicine and health services at the University of Washington School of Medicine, has not seen the ACC's recommendations.Or simply put, "how many echocardiograms does one need to read, or stress tests perform to gain advantage of a well-trained internist?"
Still, he said to be successful in getting support for a five-year general cardiology residency, the ACC would need to show what additional skill set these residents would be acquiring that they wouldn't get in internal medicine.
"Presuming they don't take on technical skills, what's left is a lot of basic general internal medicine," Dr. Fihn said. "They might be more proficient at interpreting cardiological information, but what exactly are we talking about in terms of the content?"
Just wait, soon an internal medicine career path can look like this one:
 |
|
Put Another Quarter in the Anesthesia Machine....
Grand Rounds XVII is hosted by the man behind the curtain at Waking Up Costs.
Breathe deeply his gas because next week I'm putting the blade to Grand Rounds XVIII, right here.
Please submit links in the comments section or send them directly to the Operating Room of Dr. Parker by email: cut_to_cure-at-hotmail.com. The deadline for submissions is 9:00 PM EST on Monday January 24, 2005. |
Grand Rounds XVII is hosted by the man behind the curtain at Waking Up Costs.
Breathe deeply his gas because next week I'm putting the blade to Grand Rounds XVIII, right here.
Please submit links in the comments section or send them directly to the Operating Room of Dr. Parker by email: cut_to_cure-at-hotmail.com. The deadline for submissions is 9:00 PM EST on Monday January 24, 2005. |
Monday, January 17, 2005
Tales From the Trauma Service V...
Or how hypothermia destroys the best laid plans. A young man in a MVC, initially hypertensive but after the intubation has a hypotensive episode. Responds well to the fluid challenge. Initial FAST images:

Fluid in Morrison's pouch.

None seen in the LUQ, but the spleen has an unusual appearance to it. As long as the fluid keeps going his pressure does OK. A chest tube is placed for a left pneumothorax without difficulty. Two units of packed cells transfused. BP still very labile. He is too cold for the oral thermometer to register a temp. His pH on an initial ABG is 7.10. I repeat the FAST:
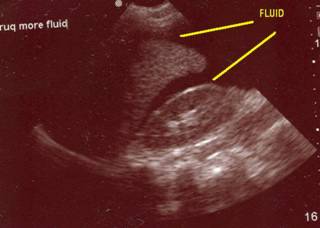
As you can see, time for the operating room. Inside there is about 1500cc of blood. The LUQ is packed off and the remainder of the abdomen explored. Liver, stomach, large and small bowel are all OK. The packs are removed from the spleen and:
The following images may be offensive!!!!
[
]
[
]
[
]
[
]
[
]
[
]
[

]
[
]
[
]
[
]
[
]
You have been warned!!!!
[
]
[
]
[
]
This patient's spleen was so pulped up that it was pretty much already dissected out:

You can see the rather pale appearing small bowel to the left. Here it is ex vivo:

He received 6 units PRBC's in the ED and OR. The spleen was out in 45 minutes but I spent another 15 pouring warm saline in his peritoneal cavity in an attempt to raise his temperature. It was raised about a degree. We took him up to the ICU and since I had no information about his brain or his aorta (he had both a first rib and scapular fracture) he was bundled up and taken to CT. The crucial cut of his chest CT:

Half of his lungs were contused. Oxygenation became increasingly difficult, and increases in PEEP were not well tolerated. His coagulopathy was profound with a PT higher than his platelet count. It would have been difficult to resuscitate him out of this, but not impossible. His family then inexplicably made him a DNR. This pretty much deflated the balloon. The residents and nurses seem to move at about three-quarter speed. He expired about five hours postop.
Or how hypothermia destroys the best laid plans. A young man in a MVC, initially hypertensive but after the intubation has a hypotensive episode. Responds well to the fluid challenge. Initial FAST images:

Fluid in Morrison's pouch.

None seen in the LUQ, but the spleen has an unusual appearance to it. As long as the fluid keeps going his pressure does OK. A chest tube is placed for a left pneumothorax without difficulty. Two units of packed cells transfused. BP still very labile. He is too cold for the oral thermometer to register a temp. His pH on an initial ABG is 7.10. I repeat the FAST:
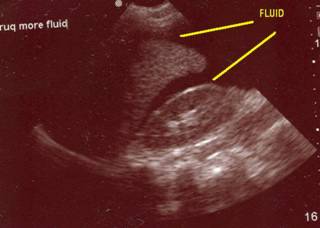
As you can see, time for the operating room. Inside there is about 1500cc of blood. The LUQ is packed off and the remainder of the abdomen explored. Liver, stomach, large and small bowel are all OK. The packs are removed from the spleen and:
The following images may be offensive!!!!
[
]
[
]
[
]
[
]
[
]
[
]
[

]
[
]
[
]
[
]
[
]
You have been warned!!!!
[
]
[
]
[
]
This patient's spleen was so pulped up that it was pretty much already dissected out:

You can see the rather pale appearing small bowel to the left. Here it is ex vivo:

He received 6 units PRBC's in the ED and OR. The spleen was out in 45 minutes but I spent another 15 pouring warm saline in his peritoneal cavity in an attempt to raise his temperature. It was raised about a degree. We took him up to the ICU and since I had no information about his brain or his aorta (he had both a first rib and scapular fracture) he was bundled up and taken to CT. The crucial cut of his chest CT:

Half of his lungs were contused. Oxygenation became increasingly difficult, and increases in PEEP were not well tolerated. His coagulopathy was profound with a PT higher than his platelet count. It would have been difficult to resuscitate him out of this, but not impossible. His family then inexplicably made him a DNR. This pretty much deflated the balloon. The residents and nurses seem to move at about three-quarter speed. He expired about five hours postop.
Labels: Tales from the Trauma Service
|Friday, January 14, 2005
Bariatric Surgery Follies.....
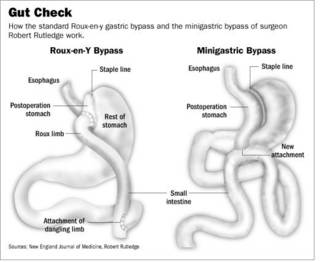
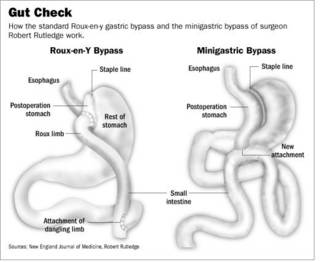
From the Wall Street Journal:A Doctor's Version Of Obesity Surgery Raises Some Bile:
The Bilroth I:

and the Bilroth II:

Both of those procedures have well-known complications such as "dumping syndrome" and "afferent loop syndrome". Ok, enough of history, back to the article:
The surgery is simpler to perform since there are fewer staple lines, as seen here in this side-by-side comparison:
It seems as if patients are trading short-term gain for long-term consequences. In reference to #19 above:
Dr. Rutledge's recent past doesn't seem reassuring:
Another great tradition, itinerant surgery. Bariatric surgery can save lives, when done properly, unfortunately many put financial gain before patent safety, both long and short-term. |
From the Wall Street Journal:A Doctor's Version Of Obesity Surgery Raises Some Bile:
In a nation of epidemic obesity, weight-loss surgery is booming. The number of such procedures, almost all of them stomach reductions, rose 36% last year to 141,000, five times the 1999 level, according to the American Society for Bariatric Surgery.Ah, the great surgical tradition of fee-splitting. Moving along:
One of the field's busiest practitioners is Robert Rutledge. Garnering patients via his Web site and local seminars, the 53-year-old surgeon charges $17,000 for his version of the surgery, undercutting the $25,000 to $30,000 typically charged for the standard procedure, known as a "gastric bypass."
Dr. Rutledge calls his variation, which is briefer and involves a shorter hospital stay, the "minigastric bypass." In the past two years, he has opened minigastric programs at hospitals in Florida, Michigan, North Carolina, California, Missouri and Arkansas.
Doctors at these sites receive training from Dr. Rutledge, who receives a portion of the fees for each surgery they do. He says about 50 minigastrics are being performed each month, with about 3,000 done since he began using the technique in 1997.
Dr. Rutledge promotes the minigastric as a safer alternative to conventional stomach reduction. Many doctors, however, say the minigastric is nearly identical to a form of weight-loss surgery that was abandoned in the 1970s because of concerns about cancer risk and the churning up of intestinal bile into the esophagus and stomach. The "reflux" of bile, an alkaline liquid secreted into the intestine that the body uses to break down fat, can produce burning chest pain and gagging and also lead to serious irritation of the esophagus.The Bilroth II gastrojejunostomy (or "Billroth") and the related Bilroth I have been a mainstay of gastric surgery for a variety of conditions for many years. Named for their inventor, Christian Albert Theodor Billroth.
As with the earlier surgery, Dr. Rutledge uses a type of hookup between the intestines and the stomach called the Billroth II. A 1985 study of 28 patients published in the journal Surgery found that those who received the Billroth II hookup had 13 times as much bile in their stomachs as patients who had conventional stomach reductions. A 2002 study of 91 patients by Japanese researchers found 31% of Billroth II patients suffered from bile refluxing into the esophagus, compared with 1.6% of patients with conventional surgery. The study appeared in the World Journal of Surgery.
The Bilroth I:

and the Bilroth II:

Both of those procedures have well-known complications such as "dumping syndrome" and "afferent loop syndrome". Ok, enough of history, back to the article:
Complicating the debate is a shortage of safety data about Dr. Rutledge's procedure. He says he tries to follow up regularly with all the patients who receive operations from him or a doctor he has trained by sending them written or e-mail questionnaires. But these methods are open to bias: People might not accurately self-report their weight or other data, and those with bad experiences might not respond to the requests for information.Dr. Parker smells something here. Look at #19 and #23 here to see what I mean. This guy seems to be leaving trouble all around:
Dr. Rutledge hasn't carried out any studies comparing his surgery to other procedures; he says that's because other surgeons have a vested interest in the status quo and refuse to participate. He has published only one article for a medical journal about his procedure. It appeared in June 2001 in Obesity Surgery and was based on data from his questionnaires.
Five doctors who practice near Dr. Rutledge's clinics say that collectively they have treated 50 patients over the past six years for side effects from the operation. "That is why no one believes his data," says one of the five, Adolfo Fernandez Jr., a professor of surgery at Wake Forest University School of Medicine. In about two dozen cases, these doctors say the patients had to have corrective surgery to undo the operations that Dr. Rutledge or one of his followers performed. About a dozen patients who have had the minigastric procedure said in interviews they suffered from bile reflux bad enough to lead to serious symptoms.
The surgery is simpler to perform since there are fewer staple lines, as seen here in this side-by-side comparison:
It seems as if patients are trading short-term gain for long-term consequences. In reference to #19 above:
Dr. Rutledge has a following of former patients who refer to him in reverential terms. Randall Edwards, a lawyer from Reno, Nev., started doing some legal work for Dr. Rutledge after having the minigastric procedure. He says he lost 158 pounds following the surgery in December 2003 and is no longer plagued by sleep apnea and other health problems from his obesity.Just wait a few years.
"This guy can save your life," he tells a group of patients awaiting surgery by Dr. Rutledge and a trainee surgeon one recent morning at the Chino Valley Medical Center, outside Los Angeles.
Another proponent is Henry Fiala, a Toronto physician who lost 117 pounds after a minigastric performed by Dr. Rutledge in 2003. Dr. Fiala has sent 20 of his patients to the U.S. for the operation, which is paid for by the government of Ontario. He is impressed by the low mortality rate reported in Dr. Rutledge's self-collected data and the quick operating time. As for bile reflux, he says: "I have a lot of patients with bile reflux and it hasn't killed them. Of all the things that go wrong, that is not the worst thing to happen."
Ms. Hanson considered the standard gastric bypass, but after finding Dr. Rutledge's Web site she decided she preferred his approach because it was less invasive. She traveled to Durham Regional Hospital in North Carolina, where Dr. Rutledge was then operating, and underwent the procedure in January 2000. It took a little under an hour, and she left the hospital two days later.See #23 above.
At first, "it was a dream come true," says Ms. Hanson. She says she quickly lost about 100 pounds, but within a year began to have attacks that started with a cold sweat followed by pain in her lower back. It felt "like someone was taking a hot dagger and just stabbing me," she says. The only relief came when she involuntarily vomited bile.
Other surgeons diagnosed the pain as bile reflux and told Ms. Hanson she needed to undergo new surgery to replace Dr. Rutledge's intestinal routing with the standard hookup. She did so in 2001 and says she hasn't had attacks since. Dr. Rutledge says he doesn't remember Ms. Hanson's case but says many doctors perform repair surgery when medication to treat the symptoms would also be effective. He says some doctors are jealous of his success and averse to innovation.
Dr. Rutledge's recent past doesn't seem reassuring:
Dr. Rutledge says he stopped performing the surgery for several months in 2001 after some patients in North Carolina complained about complications, and Durham Regional suspended its minigastric program. The North Carolina Medical Board says it investigated the complaints, but never took disciplinary action against Dr. Rutledge. He began operating again at a different hospital in Statesville, N.C., and in 2003 began his expansion into other states. He recently moved to Las Vegas, where he is opening a center later this month, but spends much of his time on the road.
Another great tradition, itinerant surgery. Bariatric surgery can save lives, when done properly, unfortunately many put financial gain before patent safety, both long and short-term. |
Thursday, January 13, 2005
The Future of Surgery IX...
Another article from General Surgery News:Initiatives Being Considered To Offer 'More Efficient' Track to Specialization:
The Powers That Be in surgery have examined this as well. In the latest Annals of Surgery:American Surgical Association Blue Ribbon Committee Report on Surgical Education: 2004:

Certainly more complicated than the current "cylindrical" or "pyramid" programs of today. Given that surgeons are some of the most dogmatic of physicians out there, if even some of this comes to fruition it will be amazing.
Another article from General Surgery News:Initiatives Being Considered To Offer 'More Efficient' Track to Specialization:
The American Board of Surgery (ABS) recently proposed the creation of a six-year primary certificate in vascular surgery, which represents the first time the board will offer a primary certificate that does not require prerequisite training and certification in general surgery. The proposal is under consideration by the initial review group of the American Board of Medical Specialties, and a decision on whether to proceed with the program is expected by the middle of next year.This is not a small move, according to a member of the American Board of Surgery:
Leaders in the fields of cardiac, breast and emergency/trauma surgery are also discussing focused training pathways, the result of a loud and growing clamor for more such specialty programs driven by factors such as the unwillingness among doctors today to train for many years, particularly female doctors, who will form an estimated 60% to 70% of the medical student body within 20 years. Currently, fully 70% of general surgery trainees eventually opt to undergo subspecialty training, and most do so by taking one to three years of fellowship training after a five-year general surgery residency. As a precedent, plastic surgery has a variety of training options, not all of which require completion of a general surgery residency.
"We need to recognize the fact that we are going to continue to need surgeons, and we have to ensure that our training programs and surgical careers are attractive to students of both genders," ABS chair Barbara Bass, MD, told General Surgery News. "We have to meet the surgical workforce needs of America, and to do that we have to come up with more efficient training pathways, albeit deliberately and thoughtfully and without sacrificing quality, or we're not going to have enough surgeons."One of those who disagree:
Dr. Bass described the decision to consider a primary certificate in vascular surgery as "a huge step, almost earthquaky" for the ABS. And the tremors have already extended to surgeons across the country, creating a huge fissure between approximately equally sized camps of those who support a continued move to reduced training time for specialists, and those who feel it may spell disaster for surgery.
For example, Gary Hoffman, MD, a colorectal and general surgeon who operates at Cedars-Sinai Medical Center in Los Angeles, is incensed by the impetus to create a variety of specialty surgical certificates.But the handwriting is on the wall and is difficult to scrub off:
"The surgeons in whose hands we now place our lives have had to spend a necessary five years learning the craft of surgery. That is why four-year general surgical residencies were eliminated years ago," Dr. Hoffman said. "What would be the ostensible purpose of even providing any general surgical training to specialty surgeons---to learn to tie a few surgical knots or to know when to place a nasogastric tube? ... This proposed lowering of our standards to fit our lifestyles may simply be a mirror of a bigger societal picture. For that analysis, however, you will need to consult a philosopher or historian. From my end of the scalpel, surgical training in all specialties needs to be strengthened, not weakened."
But Henry Kuerer, MD, who heads the Breast Surgical Oncology Training Program at M.D. Anderson Cancer Center in Houston, supports it. He holds up the plastic surgery program at Baylor College of Medicine as a shining example of a successful shortened specialty program. Residents in the Baylor program complete three years of general surgery and then three years of plastic surgery training under Saleh Shenaq, MD, professor and chief of the Division of Plastic Surgery in the Michael E. DeBakey Department of Surgery. Dr. Kuerer sees it as an excellent model for the development of similar training programs in breast surgery and other specialties.Patient demand, dear reader, will be the straw that stirs the drink not only of increased surgical specialization but of increased specialization of medicine as a whole. Some other opinions:
"We train Dr. Shenaq's residents at the third-year level in oncologic surgery and we have found them to be very, very good, and a pleasure to work with," Dr. Kuerer told General Surgery News. "My feeling is that a breast surgeon could have three years of general surgery and three years of breast oncology, which would include rotations on the multidisciplinary care of breast patients, including radiation, medical oncology, breast imaging, plastic surgery and clinical research skills."
Dr. Kuerer says patient demand is one of the seismic forces shaping this debate, as consumers become more savvy and increasingly demand treatment by breast specialists, which is making the ground tremble under the feet of some general surgeons.
"The general surgeons are concerned that even though they have appropriate surgical training and take care of breast problems, they may be shut out because patients might insist on having 'expert' surgeons with specialty training," noted Dr. Kuerer.(emphasis mine)
Others see truth to both sides of the argument. Brian Bansidhar, MD, colon and rectal surgical fellow, Lehigh Valley Hospital, Allentown, Pa., agrees that reducing the amount of general surgical training would still create specialists who are competent surgeons. However, he feels that experience outside of one's specialty area helps produce a more well-rounded surgeon.Best of luck to Dr. Bansidnar if he tries to "initiate the right treatment" without consulting an orthopedist. He and his liability carrier may need it.
"Just as an example, in my residency, we spent a month and a half doing orthopedic surgery," he said. "Did I have to do that? No. Am I going to be doing any orthopedic surgery throughout my career? No. But what that exposure did was to allow me to take trauma and general surgical patients who had orthopedic injuries, and see the big picture. Surgical issues aren't neatly compartmentalized; one problem will affect another. That being said, now I can at least better see some of the nuances and subtleties of the orthopedic injuries and initiate the right treatment, as opposed to saying, 'Well, just call orthopedics, I don't know what to do.' To say that would not be the right thing to do, nor would it be the best thing for the patient."
Kimberly Van Zee, MD, associate attending surgeon, Memorial Sloan-Kettering Cancer Center, New York City, also sees the need for a difficult, fine-linebalancing act.Dr. Van Zee's first point is taken up well by this commenter to a previous post. But the second is also valid. The number of certain cases are finite as is the hours residents are allowed to work. If proficiency is to be maintained, some early specialization will need to be allowed.
"Less exposure to general surgery would result in the surgical subspecialist being less able to treat or recognize signs or symptoms of a disorder outside of [his or her] subspecialty," she said, recognizing one argument for not changing the current training system. "But as resident work hours decrease, and the clinical experience obtained during the five-year general surgery residency decreases, an argument in favor of the earlier split arises: those who are going to continue in general surgery would be the beneficiaries of having fewer colleagues to share a limited number of the more unusual cases, thereby allowing them to complete their training with more experience."
The Powers That Be in surgery have examined this as well. In the latest Annals of Surgery:American Surgical Association Blue Ribbon Committee Report on Surgical Education: 2004:
American surgical education has a rich heritage, and its programs produce some of the best trained and most competent surgeons. Although surgery residency training has changed little since its formulation by Halsted at the beginning of the last century, surgery residency and fellowship programs continue to maintain high standards because they are highly structured, monitored, evaluated, and credentialed.The paper contains recommendations concerning medical workforce, medical student and resident education, resident workhours, faculty and professional development, and research support. The panel has the following to say about the structure of residency training:
At the dawn of the 21st Century, however, numerous forces for change are impacting medical education in general and surgical training in particular. On the one hand, the explosion of knowledge from the advances of science, systems, and information technology provide new opportunities to improve our training programs. On the other hand, as the public has become increasingly better informed about its healthcare needs and safety, its expectation has shifted and now increasingly demands advanced and specialized care. Contrary to earlier predictions of excess physicians by 2010, we appear to be on the threshold of a shortage in physician workforce. This impending shortage should be viewed in the context of Association of American Medical Colleges (AAMC) data, which show that the number of applicants to medical schools in the United States has declined by 25% since 1996. Now, nearly 50% of students entering medical school are women. The average U.S. medical student now graduates with a debt in excess of $100,000. Students of both genders are increasingly selecting specialties with more controllable lifestyles than general surgery. Furthermore, general surgery residencies experience an attrition rate of nearly 20%, primarily because of lifestyle concerns of residents. Major changes have occurred and more are foreseen in the practice of surgery. Much clinical care has moved from the inpatient hospital setting to the outpatient, and the length of stay for inpatients has significantly decreased. These shifts have resulted in a significant impact on both undergraduate and graduate medical/surgical education. Surgical care is moving from discipline-based to disease-based practice in which surgeons will increasingly practice within a team of experts. How do we train surgeons to be leaders of such multidisciplinary teams?
There are many forces driving change in the nature and structure of surgical residencies. Among these are the explosion of knowledge in all surgical fields; new technologies for teaching and assessing surgical skills and for performing surgery; evolution toward multidisciplinary collaborations in patient care; progressive subspecialization; concern for quality and safety of patient care; emphasis on professionalism and competency; and higher expectations of patients. Regulatory changes have limited allowable work hours by residents and put additional stress on the ability to meet the service needs of hospitals as educational needs are given priority.To that end the authors put forth a suggested structure of training that looks like an organizational chart for a government bureaucracy:
Today's surgical resident is a different person. There are more women in surgical training, and residents have more education-related debt. Residents have greater concerns about their lifestyle and length of training. There is need to maximize efficiencies and minimize the duration of residency.
It is increasingly apparent that as subspecialization in surgery continues to evolve and the appeal of broad general surgical practice diminishes, the illusion that a uniform training program purporting to produce competence in all areas is fading. One size no longer fits all. Uncommon case materials are less efficiently distributed when they are used to train individuals whose ultimate goals do not involve focus in these areas. Education research is pushing toward competence-based advancement, replacing time-in-service.
Subspecialty fellowship training is at present largely unregulated, unsupervised, nonuniform, and uncertified. Research by residents during residency is too often for the sole purpose of attaining a clinical fellowship or to meet the needs of faculty for laboratory workers.
A new paradigm is needed that promotes both the varieties of general surgical practice and the subspecialties that derive from general surgery. This training paradigm must achieve greater efficiency and use different methods to be able to accommodate the changing needs of surgical residents and surgery as it will be practiced.
Recommendations
1. Surgical residencies should be restructured to ensure that all trainees receive a common grounding in basic principles of surgical disease and patient care.
2. There needs to be acceptance of the reality that most surgeons will confine the scope of their practices to meet definable goals. This should lead to earlier differentiation into goal-oriented specialty tracks.
3. New teaching technologies (ie, simulators, virtual reality) and verification of competence at each training milepost should be introduced as they become validated and available. A goal should be to define a curriculum for surgical skills that must be acquired by surgical trainees outside the operating room before they begin to operate on patients.
4. It is suggested that a modular format be developed to include a basic surgical core curriculum, and further training in either general surgery or a surgical subspecialty leading to the relevant, specific certification.
5. Furthermore, focused subspecialization would be available through postgraduate fellowships (ie, breast, endocrine, HPB, congenital heart, hand).
6. An optional research module of not less than 2 years can either be interposed between the basic and advanced modules or taken at completion of the residency/fellowship for career development in conjunction with a first faculty position.
7. The option to study for completion of an advanced graduate degree (PhD, MPH, MBA) may occur either after the basic module or after residency.
8. Design, supervision, and certification of the new curricula and the training programs in which they will be used will remain the domain of the respective Boards, RRCs, and surgical specialty societies.
9. It is understood that there will be manifold logistic challenges to implementation, including acceptance by the various stakeholders
(emphasis mine)

Certainly more complicated than the current "cylindrical" or "pyramid" programs of today. Given that surgeons are some of the most dogmatic of physicians out there, if even some of this comes to fruition it will be amazing.
Labels: Future of Surgery
|Wednesday, January 12, 2005
Placed on Retainer....
I have added the medical blogosphere's favorite lawyer (and commenter): Curious JD. His presence will add greatly to the tort reform debate. |
I have added the medical blogosphere's favorite lawyer (and commenter): Curious JD. His presence will add greatly to the tort reform debate. |
The Creeping Specialty Scourge II.....
From this week's New England Journal of Medicine:The Emergence of Physician-Owned Specialty Hospitals:
Hospitals are beginning to fight back:
As I posted earlier the Big Hospital was considering such "economic credentialing" measures to "insure solvency". Such requirements would include:
Disclosure of any "financial relationship" with another hospital which would include"investment interest....contractual relationships...and any other remuneration". The existence of such could result in the termination of privileges or a prohibition on holding medical staff office.
The practice of "proportional admissions". That is, the payer mix of your practice should match your admitting profile to Big Hospital. If you "fall off the curve" you would be required to provide practice records for analysis.
A "pre-application" process which may involve a "pre-application" interview. The "pre-application" form has questions about "financial relationships" with other hospitals as well as questions about "plans for performing procedures in your office that would usually be performed in the hospital". So not only will the hospital look askance if you are a shareholder in a hospital or ambulatory surgery center, they will also take issue if you, as many plastic surgeons and gastroenterologists do, have equipment and staff to perform procedures in your own office. The real beauty of this approach is the legal sleight-of-hand concerning the "pre-application". Under regulations if a physician's application is denied, they are entitled to a hearing and appeals and the whole due process thing. All avoided by the "pre-application" use. Clever, isn't it?
I hope I have enough blood in my finger to sign this when it comes across my desk.
Serving on multiple hospital committees I can appreciate the situation the hospital is in. They lose the high-dollar procedures to the specialty hospitals and they get the sickest patients. The only leverage the hospital has is to place conditions on staff participation. This has managed care implications as well since some plans have exclusive contracts with certain hospitals. So if you're not on staff you cannot participate in the plan. OTOH the measures described above seem quite Orwellian to me. Of course the true test of these measures won't be the up-or-down vote of the board or medical staff, it will lie in if and when they are used. A paper tiger? Time will tell.
|
From this week's New England Journal of Medicine:The Emergence of Physician-Owned Specialty Hospitals:
In 1972, the federal government, no longer satisfied that America's social contract with its physicians could be shaped by self-regulation alone, began to weave a complex web of laws and regulations circumscribing the business practices of doctors. As a consequence, the government, with very few exceptions, prohibits physicians from referring their Medicare and Medicaid patients to freestanding entities in which a practitioner or a member of the practitioner's immediate family has an investment interest. One of these exceptions, known as the "whole-hospital exception," has become the subject of a serious dispute, because general hospitals strongly object to the use of this exception by physicians who refer their patients to specialty hospitals in which these practitioners hold an ownership interest.The specialty hospital numbers are increasing, for many reasons:
Although most of the specialty hospitals that have opened since 1990 are located in only a few states, the number of such hospitals has tripled nationally, to some 100 facilities. This rapid growth has raised concerns among general hospitals, which consider the specialized facilities an unfair form of competition as they currently operate that should be outlawed. Recognizing these concerns, in December 2003 Congress declared a moratorium of 18 months on the development of new specialty hospitals that are partly owned by physicians who refer their patients to them and directed two federal agencies to study the effect of these facilities on the health care system.
The specialty hospitals are part of a large movement that is roiling relations between general hospitals and physicians throughout the country - the shifting of patients to alternative settings. The number of ambulatory-surgery centers, diagnostic testing facilities, and specialty hospitals has steadily increased during the past 15 years as physicians, taking advantage of new forms of technology, available capital, and supportive health policies, pursue new ventures outside hospitals and their control. Also propelling this shift to alternative settings is the view held by many physicians that hospitals are not responsive to physicians' demands for a larger voice in the governance of the hospitals. Other factors that have energized physicians are the ongoing consolidation of private health care insurers into ever larger enterprises and the hospital mergers that are increasing the market muscle of general hospitals in a growing number of communities.The hospitals are seen by many as a bully and specialty/physician-owned facilities are seen as a way to exercise control. The growth is confined to a few states that do not have certificate-of-need laws:
In a 2003 report requested by Congress, the GAO counted 100 specialty hospitals in 28 states and an additional 26 entities under development About two thirds of the specialty hospitals in operation or under development are located in just seven states: Arizona, California, Kansas, Louisiana, Oklahoma, South Dakota, and Texas. Most of these facilities (85 percent) are in rapidly growing urban areas, although only 43 percent of those that have opened since 1990 are in such areas. Virtually all specialty hospitals -96 percent of those built since 1990 - are in states that do not require the developers to secure a "certificate of need," which is a permit that is issued by states before a health care facility may be constructed or expanded.Supporters of such facilities tout their competitive advantages:
The GAO also reported that more than 90 percent of the specialty hospitals that have opened since 1990 are for-profit entities, as compared with 20 percent of all general hospitals. Specialty hospitals are much less likely than general hospitals to have emergency departments (45 percent vs. 92 percent) or to treat Medicaid or uninsured patients. In 2001, specialty hospitals accounted for an estimated $871 million, or 1 percent, of Medicare's spending on inpatient services, nearly two thirds of which went to facilities that treat patients with cardiac disorders .
Physicians practicing at both types of facilities told us that they can perform about twice as many cases in a given time period at specialty hospitals as at community hospitals. Physicians mentioned operating room turnaround times at specialty hospitals of 1020 minutes, compared with over an hour at the community hospitals where they also practice. . . . Surgeons at one specialty hospital told us about working between two operating rooms at once to increase their productivity. At one specialty hospital, we were told that physician incomes had increased by 30 percent as a result of increased productivity........
......Even the possibility of the development of a specialty hospital in a particular market can have a strong influence on the reactions of general hospitals A case in point is the city of Indianapolis, 1 of 12 cities or counties that have been studied closely over the past decade by the Center for Studying Health System Change, a nonprofit research organization supported by the Robert Wood Johnson Foundation. One of the center's analysts, Kelly J. Devers, described the scene in Indianapolis at a conference in Washington, D.C., on April 15, 2003:
The building boom began when specialists affiliated with one of the four major (nonprofit) hospital systems threatened to partner with MedCath. . . . These physicians had pressed the system to build a new hospital in which they could share ownership interest but were turned away. The new competitive threat posed by a heart hospital jointly owned by its cardiologists and MedCath convinced the system to build a freestanding heart hospital, and the physicians own up to a 30-percent share. Another hospital system also bent under pressure from specialists who threatened to partner with MedCath, agreeing to build a new freestanding facility in which they could own up to 50 percent. Given the increased competition from specialty heart hospitals and the MedCath threat, the two remaining large hospital systems in the market built their own heart hospitals, but without physician ownership.
Hospitals are beginning to fight back:
General hospitals have also responded in other ways to physicians who shift, or threaten to shift, their patients to a specialty hospital. The general hospitals have sought to deny admitting privileges to physicians who become part owners of a nearby specialty hospital (a practice known as economic credentialing) or have denied them promotions. Some courts have upheld these actions, but there are cases pending. Devers reported that general hospitals have also attempted to discourage health care plans from contracting with specialty hospitals "by threatening to terminate their contracts for all of the hospitals in the system and all of the services."As stated above the courts are still sorting out the "restraint of trade" issues.
As I posted earlier the Big Hospital was considering such "economic credentialing" measures to "insure solvency". Such requirements would include:
Disclosure of any "financial relationship" with another hospital which would include"investment interest....contractual relationships...and any other remuneration". The existence of such could result in the termination of privileges or a prohibition on holding medical staff office.
The practice of "proportional admissions". That is, the payer mix of your practice should match your admitting profile to Big Hospital. If you "fall off the curve" you would be required to provide practice records for analysis.
A "pre-application" process which may involve a "pre-application" interview. The "pre-application" form has questions about "financial relationships" with other hospitals as well as questions about "plans for performing procedures in your office that would usually be performed in the hospital". So not only will the hospital look askance if you are a shareholder in a hospital or ambulatory surgery center, they will also take issue if you, as many plastic surgeons and gastroenterologists do, have equipment and staff to perform procedures in your own office. The real beauty of this approach is the legal sleight-of-hand concerning the "pre-application". Under regulations if a physician's application is denied, they are entitled to a hearing and appeals and the whole due process thing. All avoided by the "pre-application" use. Clever, isn't it?
I hope I have enough blood in my finger to sign this when it comes across my desk.
Serving on multiple hospital committees I can appreciate the situation the hospital is in. They lose the high-dollar procedures to the specialty hospitals and they get the sickest patients. The only leverage the hospital has is to place conditions on staff participation. This has managed care implications as well since some plans have exclusive contracts with certain hospitals. So if you're not on staff you cannot participate in the plan. OTOH the measures described above seem quite Orwellian to me. Of course the true test of these measures won't be the up-or-down vote of the board or medical staff, it will lie in if and when they are used. A paper tiger? Time will tell.
|
Tuesday, January 11, 2005
Cherry Picking in New York State....
No, not a tourist attraction, but the rearing up of the ugly head of unintended consequences. From The New York Times:Cardiologists Say Rankings Sway Choices on Surgery:
You think?
Many are leery of such "scorecards" because they don't believe that adequate allowances are made for the very sick patients who can affect the numbers. The difference in morbidity and mortality between an elective angioplasty and an emergent one is impressive:
No, not a tourist attraction, but the rearing up of the ugly head of unintended consequences. From The New York Times:Cardiologists Say Rankings Sway Choices on Surgery:
An overwhelming majority of cardiologists in New York say that, in certain instances, they do not operate on patients who might benefit from heart surgery, because they are worried about hurting their rankings on physician scorecards issued by the state, according to a survey released yesterday.So eight out of ten believe that patients are denied potentially lifesaving procedures and almost as many admit that the scorecard had influenced their clinical decision making.
The survey, which was sponsored by the School of Medicine and Dentistry at the University of Rochester, demonstrated the difficulty that many doctors have with the public disclosure of their performance data, an idea pioneered by New York State. In 1994, the state's Department of Health began to compile data on cardiologists performing coronary angioplasty, a less invasive procedure than bypass surgery for restoring blood flow to the heart.
Eighty-three percent of the cardiologists surveyed said that because the state reports the mortality rates of heart surgeons, patients who might benefit from angioplasty may not receive the procedure. In addition, 79 percent of the doctors said that the knowledge that mortality statistics would be made public had, at times, influenced their decision on whether to operate.
You think?
Many are leery of such "scorecards" because they don't believe that adequate allowances are made for the very sick patients who can affect the numbers. The difference in morbidity and mortality between an elective angioplasty and an emergent one is impressive:
Angioplasty, when performed as elective surgery, has a mortality rate of less than 1 percent. But when patients come to the hospital as they are suffering a heart attack, when their bodies are in shock and blood pressure is low, there is a 60 percent chance that they will die, Dr. Narins said. The chance of survival can be increased to 50 percent if surgery is performed.If the numbers Dr. Narins quotes are correct, the physician is looking at a ten percent increase of survivability, but only up to the degree of a coin flip. "Why risk my scorecard and liability premium over a patient who is likely to die anyway?" Shocking? Uncaring? perhaps, but to 80 percent of New York cardiologists it is a reality. |
The Naked Monarch....
The Mad House Madman has put forth an excellent series of posts about his conflict concerning the decline of a giant. His story brought back memories from residency when I (and others) were put in a similar position, the position of keeping the attendings out of trouble.
The trouble was not so much due to senility, as the hospital where I trained would require surgeons to hang up the scalpel at age 65. The trouble we would need to be on the lookout for was due to incompetence and buffoonery.
There were always private attendings who would only perform high-risk surgeries on sick patients at the University Hospital while doing the bread-and-butter outpatient stuff at the community hospital. That was OK as far as I was concerned, the medical care of the very sick is what the University Hospital was for.
A less palatable situation was the CV surgeon who was such an ass that none of the others in his section or their PA's would scrub with him. So a resident, sometimes even a PGY 4 would hold hook for this guy while he insulted them the whole case.
There was the oft-sued specialist surgeon who was on-and-off of double-secret probation for a wide variety of offenses. His wife was a powerful physician at the University hospital who would throw her weight around to keep him on staff. He would perform operations he had no business doing and demand a resident scrub with him. The upper levels would conveniently find something else to do and the hapless intern would find himself in a very uncomfortable situation. After a few months of his latest return to staff we approached our chairman and program director with our concerns. We had short, medium, and long-term concerns.
Short-term was the immediate risk to the patient, medium-term was the discomfort of a M&M presentation (under the rules one could not say "That clown who had no business in the operating room wouldn't listen to me!!"), and long-term was the lawsuit that would follow you around for time immemorial. We told them that we as residents could do little about the first but we could do something about the last. With the support of one of the attendings we took the bold move of telling our chairman the we respectfully refused to scrub with this surgeon again. Our gamble paid off and we avoided both termination as well as avoided participating in his cases.
He later was removed from the staff for more of the same.
Looking back it amazes me that the faculty and hospital would go to such lengths to protect such an incompetent surgeon. They would even go so far as to question our motivation and competence.
Physicians tend to bend over backwards to protect another from the consequences of their actions. We would "cover up" problems with drugs and alcohol, affairs, and issues of competence. Why? It was easy to sweep it under the rug, and mostly, no harm was done. Other physicians, both attending and housestaff, would make sure things were OK.
But the rules changed.
Physicians realize that no one gains from such "enabling" behavior. The patients continue to suffer, the impaired physician does not get the help they need, and the rest of the physicians run the risk of suit as well as increased premiums for themselves.
The "enablers" realize that the cost of their duplicity is too high.
So the tolerance for such behaviors is much less, but pointing them out is no easier. |
The Mad House Madman has put forth an excellent series of posts about his conflict concerning the decline of a giant. His story brought back memories from residency when I (and others) were put in a similar position, the position of keeping the attendings out of trouble.
The trouble was not so much due to senility, as the hospital where I trained would require surgeons to hang up the scalpel at age 65. The trouble we would need to be on the lookout for was due to incompetence and buffoonery.
There were always private attendings who would only perform high-risk surgeries on sick patients at the University Hospital while doing the bread-and-butter outpatient stuff at the community hospital. That was OK as far as I was concerned, the medical care of the very sick is what the University Hospital was for.
A less palatable situation was the CV surgeon who was such an ass that none of the others in his section or their PA's would scrub with him. So a resident, sometimes even a PGY 4 would hold hook for this guy while he insulted them the whole case.
There was the oft-sued specialist surgeon who was on-and-off of double-secret probation for a wide variety of offenses. His wife was a powerful physician at the University hospital who would throw her weight around to keep him on staff. He would perform operations he had no business doing and demand a resident scrub with him. The upper levels would conveniently find something else to do and the hapless intern would find himself in a very uncomfortable situation. After a few months of his latest return to staff we approached our chairman and program director with our concerns. We had short, medium, and long-term concerns.
Short-term was the immediate risk to the patient, medium-term was the discomfort of a M&M presentation (under the rules one could not say "That clown who had no business in the operating room wouldn't listen to me!!"), and long-term was the lawsuit that would follow you around for time immemorial. We told them that we as residents could do little about the first but we could do something about the last. With the support of one of the attendings we took the bold move of telling our chairman the we respectfully refused to scrub with this surgeon again. Our gamble paid off and we avoided both termination as well as avoided participating in his cases.
He later was removed from the staff for more of the same.
Looking back it amazes me that the faculty and hospital would go to such lengths to protect such an incompetent surgeon. They would even go so far as to question our motivation and competence.
Physicians tend to bend over backwards to protect another from the consequences of their actions. We would "cover up" problems with drugs and alcohol, affairs, and issues of competence. Why? It was easy to sweep it under the rug, and mostly, no harm was done. Other physicians, both attending and housestaff, would make sure things were OK.
But the rules changed.
Physicians realize that no one gains from such "enabling" behavior. The patients continue to suffer, the impaired physician does not get the help they need, and the rest of the physicians run the risk of suit as well as increased premiums for themselves.
The "enablers" realize that the cost of their duplicity is too high.
So the tolerance for such behaviors is much less, but pointing them out is no easier. |
Monday, January 10, 2005
TennCare Lives!!!
From the Nashville Tennessean:TennCare preserved but scaled back, governor says:
The Governor's own web site has more, including something for the citizens of "fairyland"
It will be entertaining to see how this plays out, how a statewide medical plan cuts benefits to maintain solvency.
Will it be a floor or a ceiling? |
From the Nashville Tennessean:TennCare preserved but scaled back, governor says:
Gov. Phil Bredesen announced today that he has preserved the TennCare program for the poor and uninsurable.
The program will be scaled back, from 1.3 million users to about 1 million. But that scaling back will affect only adults – children have been spared removal from TennCare's rolls, he said.
''This is a huge victory on behalf of Tennessee's children,'' Bredesen said.
TennCare is a state plan that expands on the federal Medicaid program. Adults in that expanded population will no longer get service, Bredesen said. But about 612,000 children now covered will continue to be covered, he said.
Bredesen criticized advocates and lawyers for patients for not accepting fiscal reality for the past two months, saying they are ''living in a fairyland'' in insisting on the kind of coverage Tennessee now provides.
The Governor's own web site has more, including something for the citizens of "fairyland"
The plan for “basic TennCare” preserves full coverage for all 612,000 children on the program and maintains a reasonable level of benefits for 396,000 adults who are eligible for Medicaid, the state and federal program for individuals and families with low incomes. As many as 323,000 adults who are not eligible for Medicaid will lose TennCare coverage — although 24% of those enrollees still will be covered under Medicare, the federal program for people who are older or who have disabilities. The State still could maintain limited care for some enrollees losing coverage if it succeeds in challenging legal constraints that public-interest attorneys have placed on the program over the years.
It will be entertaining to see how this plays out, how a statewide medical plan cuts benefits to maintain solvency.
Will it be a floor or a ceiling? |
The Future of Surgery VIII......
From General Surgery News:Details of the ABS Proposal For a Primary Certificate In Vascular Surgery
I couldn't find anything on the American Board of Surgery Website about this. I have posted on the desire of vascular surgeons to have their own board before and think that it is a good thing for the vascular surgeons. It will allow those who wish to specialize only in vascular surgery to do so without "wasting their time" performing general surgical cases. This would also allow the scarce general surgery cases to go to those who could benefit from them.
A disadvantage would be the loss of the "well-rounded" surgeon. This is a flimsy argument given the data about the effects of training and volume on results for certain procedures.
Of course, for the forseeable future, most of these specialists would be confined to the academic center or major metropolitan area. So you may need to travel to cure your ills.
From General Surgery News:Details of the ABS Proposal For a Primary Certificate In Vascular Surgery
Candidates for this certificate will be required to complete six years of integrated training, including approximately three years of general surgery and another three of vascular surgery training.
Upon completion, the surgeon would be eligible for certification in vascular surgery by the Vascular Surgery Board of the American Board of Surgery (VSB-ABS) and would not be eligible for certification in general surgery.
The curriculum for the project has been developed by the Association of Program Directors in Vascular Surgery and the VSB-ABS.
The ABS's proposal "recognizes the significant evolution in vascular surgery as a technically distinct specialty in surgery over the last decade," said ABS chair Barbara Bass, MD. "The novel approaches more widely used in vascular surgery, including endovascular procedures and the decrease in abdominal procedures, has led the vascular surgery community to support development of a training pathway for a surgeon whose practice would be exclusively in the field of vascular surgery," she added.
I couldn't find anything on the American Board of Surgery Website about this. I have posted on the desire of vascular surgeons to have their own board before and think that it is a good thing for the vascular surgeons. It will allow those who wish to specialize only in vascular surgery to do so without "wasting their time" performing general surgical cases. This would also allow the scarce general surgery cases to go to those who could benefit from them.
A disadvantage would be the loss of the "well-rounded" surgeon. This is a flimsy argument given the data about the effects of training and volume on results for certain procedures.
Of course, for the forseeable future, most of these specialists would be confined to the academic center or major metropolitan area. So you may need to travel to cure your ills.
Labels: Future of Surgery
|Sunday, January 09, 2005
Hail to the Chief....
Excerpts from President Bush's' speech last week in Illinois:President Discusses Medical Liability Reform. Starts off with the list of local dignitaries, move on to discussion of medical savings accounts, medical informatics, and tsunami relief. Then to the meat of the speech:
Joint and several liability reform may have more of a long-term impact than caps would. Hopefully it will be a good year for tort reform at the state and federal level. |
Excerpts from President Bush's' speech last week in Illinois:President Discusses Medical Liability Reform. Starts off with the list of local dignitaries, move on to discussion of medical savings accounts, medical informatics, and tsunami relief. Then to the meat of the speech:
Many of the costs that we're talking about don't start in an examining room or an operating room. They start in a courtroom. (Applause.) What's happening all across this country is that lawyers are filing baseless suits against hospitals and doctors. That's just a plain fact. (Applause.) And they're doing it for a simple reason. They know the medical liability system is tilted in their favor. (Applause.) Jury awards in medical liability cases have skyrocketed in recent years. That means every claim filed by a personal injury lawyer brings the chance of a huge payoff or a profitable settlement out of court. That's what that means. Doctors and hospitals realize this. They know it's expensive to fight a lawsuit, even if it doesn't have any merit. And because the system is so unpredictable, there is a constant risk of being hit by a massive jury award. So doctors end up paying tens of thousands, or even hundreds of thousands of dollars to settle claims out of court, even when they know they have done nothing wrong.I'm sorry Mr. President that's not quite true. Many times physicians are in a situation where they cannot pass on their increased costs to patients. I believe that if a "premium surcharge" was allowed that the populace at large would not passively sit by. Since the crisis would affect them directly, they would take more notice.
That's what's happening in the system today. It's a system that's just not fair. It's costly for the doctors; it's costly for small businesses; it's costly for hospitals; it is really costly for patients. (Applause.)
When those providing insurance have to pay the bills for enormous jury verdicts or out-of-court settlements, they have to raise premiums on physicians they cover. Specialists in high-risk practices like OB/GYN or neurosurgery are particularly vulnerable to lawsuits. So their premiums rise the fastest. You're about to hear a couple of stories of folks in this area who can testify to that fact.
Because junk lawsuits are so unpredictable, they drive up insurance costs for all doctors, even for those who have never been sued; even for those who have never had a claim against them. When insurance premiums rise, doctors have no choice but to pass some of the costs on to their patients. That means you're paying for junk lawsuits every time you go to see your doctor. That's the effect of all the lawsuits. It affects your wallet. If you're a patient, it means you're paying a higher cost to go see your doctor. If part of the national strategy has got to be to make sure health care is available and affordable, health care becomes less affordable because of junk lawsuits.
In 2003, almost half of all American hospitals lost physicians or reduced services because of medical liability concerns. Think about that. One-half of all American hospitals lost physicians. Over the past two years, the liability crisis has forced out about 160 physicians in Madison and St. Clair Counties alone. When doctors move or close their practices, guess who suffers. The patients; the people who live in these good town in this part of the world. Pregnant women have to travel longer distances for checkups. Accident victims lose critical minutes in transit to faraway emergency rooms. New residents, people you're trying to get to come and live in your communities have a hard time finding doctors willing to accept extra patients. And that causes the quality of life in your community to deteriorate. It's a problem that we must address.The President then points out several physicians, patients, and hospital administrators out of the audience and tells their stories. Stories of physicians and hospitals cutting back on services, and patients feeling the effects of those cutbacks. All due to liability insurance premium increases.
America's health care professionals should be focused on fighting illnesses, not on fighting lawsuits. (Applause.) Junk lawsuits change the way docs do their job. Instead of trying to heal the patients, doctors try not to get sued. Makes sense, doesn't it? If you're worried about getting sued, you're going to do everything you can to make sure you don't get sued. That's why doctors practice what's called defensive medicine. That means they're writing prescriptions or ordering tests that really aren't necessary, just to reduce the potential of a future lawsuit.
They have specialists who stop taking emergency room calls. Doctors turn away patients with complicated, life-threatening conditions because they carry the highest risk for a lawsuit. Defensive medicine drives a wedge between the doctors and the patients, and defensive medicine is incredibly costly for our society. Altogether, defensive medicine drains some $60 billion to $100 billion from the economy. Defensive medicine raises medical bills for patients and increases insurance costs for employers and it takes money away that small businesses could use to invest and expand.
But the other thing I discovered is that because of medical liability problems and lawsuits and increasing premiums and the defensive practice of medicine, your federal budget spends $28 billion a year extra money. See, we have to pay for Medicaid and Medicare and veterans' benefits. The rising cost of health care, the number of lawsuits, the defensive practice of medicine is driving up the cost to our taxpayers. Medical liability reform is a national issue and it requires a national solution. (Applause.)
So I went to Congress with some proposals that I think are fair, proposals that will build confidence in the judicial system. Nobody likes to come to a part of the world that says the judicial system is out of control and people lose confidence in it. We've got to have confidence in the fairness of our system. We want people who are harmed to be able to get -- have their day in court and get fair treatment in the courts of law. But we want -- we don't want a system that's so tilted the other way that it runs good doctors out of business and makes it hard for hospitals to deliver care.
I believe a victim of a legitimate medical error should be allowed to collect full economic damages, 100 percent of the cost of their medical care and recovery, plus economic losses for the rest of their life. Seems to be fair, if you get hurt. (Applause.) And when appropriate, injured people should be allowed to collect reasonable non-economic damages. And in the case of truly egregious wrongdoing, patients should be entitled to punitive damages. But there needs to be some reason, when it comes to non-economic damages in the system, and that's why I proposed a hard cap of $250,000 on non-economic damages. (Applause.)
Interestingly enough, the state of California has a cap on non-economic damages that was enacted in 1975. Patients in that state see their claims settled a third faster than states without those limits. In other words, patients are treated more fairly where there's a cap. And since 1975, insurance premiums for California doctors have become much more affordable premiums than anywhere else in the country -- than in most states. Caps on non-economic damages work. It's a good idea and the Congress ought to adopt them. (Applause.)
We have another problem with our legal system, and that is trial lawyers sometimes sue all the doctors involved in the patient's case even if most of the doctors have nothing to do with the patient's injuries. It's simply unfair to punish doctors who have done nothing wrong. (Applause.) And so, to make sure doctors and hospitals are treated fairly, Congress needs to pass joint and several liability reform. (Applause.)
Joint and several liability reform may have more of a long-term impact than caps would. Hopefully it will be a good year for tort reform at the state and federal level. |
Wednesday, January 05, 2005
More Gasoline on the Fire....
I certainly seem to have stirred up a hornet's nest with this post about the pathology report. I haven't gotten such a response since this post in October of 2003. The comments have gone down a "party line" with physicians being supportive and patients taking issue with my position. The comments have provided an interesting debate on the "ownership" of medical records and lab results. I was ready to move on to other things but I was accused by Trapper of Issemmelweis of "slamming a cancerous woman". I don't recall revealing the results in the post. They were benign, by the way.
The facts:
The patient knew that she would have to return to the office for a follow-up to discuss results, check the wound, and review follow up plans.
She knew her insurance company required a co-pay. I was contractually required to collect it.
She refused to pay it and demanded the results over the phone, against my office policy.
She wanted her results faxed to her gynecologist who referred her my office staff complied.
It was made clear that if she wanted her records with the report, she was welcome to a copy of her records. It was made clear to her that she would be required to pay for the copy. Rates for medical record copying in Georgia are set by law.
She got what she wanted, her path report. I dismissed her for the rude treatment she showed my office staff as well as the litigation threat.
She knew the rules, but when it came time to follow them, she didn't want to.
How was she "slammed" by me? |
I certainly seem to have stirred up a hornet's nest with this post about the pathology report. I haven't gotten such a response since this post in October of 2003. The comments have gone down a "party line" with physicians being supportive and patients taking issue with my position. The comments have provided an interesting debate on the "ownership" of medical records and lab results. I was ready to move on to other things but I was accused by Trapper of Issemmelweis of "slamming a cancerous woman". I don't recall revealing the results in the post. They were benign, by the way.
The facts:
The patient knew that she would have to return to the office for a follow-up to discuss results, check the wound, and review follow up plans.
She knew her insurance company required a co-pay. I was contractually required to collect it.
She refused to pay it and demanded the results over the phone, against my office policy.
She wanted her results faxed to her gynecologist who referred her my office staff complied.
It was made clear that if she wanted her records with the report, she was welcome to a copy of her records. It was made clear to her that she would be required to pay for the copy. Rates for medical record copying in Georgia are set by law.
She got what she wanted, her path report. I dismissed her for the rude treatment she showed my office staff as well as the litigation threat.
She knew the rules, but when it came time to follow them, she didn't want to.
How was she "slammed" by me? |
The Cop on the Beat...
From the New York Times today: Panel Seeks Better Disciplining of Doctors
As has been pointed out before a few bad apples are ruining the whole bunch:
Perhaps state boards could devote more time and effort to quality assurance and less time on junk like this.
The boards need to step forward because of the obstacles placed in the way of medical staff intervention concerning quality of care.
Now in what may be described as the alter-ego of the infamous DoctorsKnow a site which "unmasks" the evil among us:Questionable Doctors has data about the number of "Serious Doctor Disciplinary Actions" by state medical boards. |
From the New York Times today: Panel Seeks Better Disciplining of Doctors
Experts retained by the Bush administration said on Tuesday that more effective disciplining of incompetent doctors could significantly alleviate the problem of medical malpractice litigation.
As President Bush prepared to head to Illinois on Wednesday to campaign for limits on malpractice lawsuits, the experts said that states should first identify those doctors most likely to make mistakes that injure patients and lead to lawsuits.
As has been pointed out before a few bad apples are ruining the whole bunch:
Randall R. Bovbjerg, a researcher at the Urban Institute, said, "If you take the worst performers out of practice, that will have an impact" on malpractice litigation. "Most doctors have few or no claims filed against them," he added. "But within any specialty, a few doctors have a high proportion of the claims."Medical boards have been more aggressive over time,doing a difficult job:
The boards usually have small budgets and small numbers of employees to cope with thousands of complaints each year, he said. Moreover, he said, revoking an incompetent doctor's license can take months or years and cost a great deal, especially if the case goes to a full hearing before a board of examiners.Medical boards have extensive due process provisions, because if you lose a license in one state it is virtually impossible to keep, much less obtain, a license. Massachutsetts is cited as an example to follow:
State medical boards took 5,230 disciplinary actions against doctors in 2003, according to the Federation of State Medical Boards, the national umbrella group for the state agencies. The total was up 7 percent from 2002 and up 41 percent from 1993.
Without waiting for a complaint to be filed, the Massachusetts Board of Registration in Medicine conducts a clinical review of any doctor who has made three or more malpractice payments to patients as a result of jury verdicts or settlements.In Georgia if you have a judgment or settlement of over $100,000 the Board of Medical Examiners gets involved, regardless of previous claim history.
Nancy Achin Audesse, executive director of the board, said: "Three is a magic number. Doctors who have to make three or more payments are also more likely to be named in consumer complaints and to be subject to discipline by hospitals and the medical board."
In Massachusetts in the last 10 years, Ms. Audesse said, "one-fourth of 1 percent of all the doctors - 98 of the 37,369 doctors - accounted for more than 13 percent of all the malpractice payments, $134 million of the $1 billion in total payments."
Perhaps state boards could devote more time and effort to quality assurance and less time on junk like this.
The boards need to step forward because of the obstacles placed in the way of medical staff intervention concerning quality of care.
Now in what may be described as the alter-ego of the infamous DoctorsKnow a site which "unmasks" the evil among us:Questionable Doctors has data about the number of "Serious Doctor Disciplinary Actions" by state medical boards. |

USC 55 Oklahoma 19
The Trojans beat the Sooners so bad that you expected the piano finale from Layla to be in the background. Of course around here the populace is clamoring for the Auburn Tigers to get a piece of the national title.
So college football is over, much to my chagrin.

Starting up 2005 for the Dogs:Boise State. |
Tuesday, January 04, 2005
Tales From the Trauma Service IV....
This is one of those cases that if I never see one again during my career it will be too soon. Be warned, some of the images are very disturbing.
20-ish restraint status unknown driver in a single vehicle collision. Questionable loss of consciousness. Impressive finding on physical exam (which I will reveal later). Some select views of his CT scans:

Air surrounding the right kidney and a questionable pneumoperitoneum:

Even more air. Here are some images from the CT of his lumbar spine:
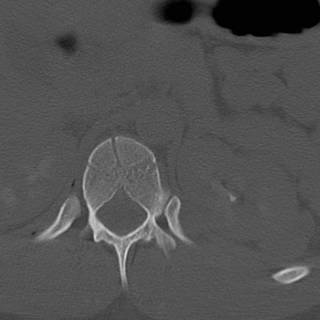

Appears to be a L1 compression fracture on the reconstruction.

Ouch!! So off we go to the OR for bilateral chest tubes (he had bilateral pneumothoracies on CT) exploratory laparotomy and reconstruction of his abdominal wall. The following images may not be suitable for all viewers:
[
]
[
]
[
]
[
]
[
]
[
]
[

[
]
[
]
[
]
[
]
[
]
[
OK YOU WERE WARNED!!!!
[
]
[
]
Here is how he presented to the ED. This photo was taken in the OR after application of a betadine scrub:
 From the left.
From the left.

And from the right. The most medial tissue seen in the left-sided incision is the posterior rectus sheath. Moving along:

Here are the right and left inferior portions of the rectus muscles. Remember this was done during the collision, probably by the seat belt. The superior portions had retracted upward.

The cecum is to the patient's right. Highlighted is a portion of denuded small bowel. Several other mesenteric tears were found in the last 21/2 feet of small bowel. The overlying bowel was intact and appeared to be perfused. This was confirmed by a Wood's lamp exam after injection of fluorescein. The segment pictured above was resected and an ileocolic anastomosis performed. Did a rather extensive lookaround. The duodenum was Kocherized and both kidneys were reflected medially. It was then time to put his abdominal wall back together.
The skin and subq fat were separated along the left flank posteriorly that I felt the tips of the 11th and 12th ribs. It extended to the posterior axiilary line on the right. The transversalis and oblique muscles had been divided on the left. I reapproximated them using their fascial layers to hold the suture. There was no good way to reapproximate the rectus since the muscle would not hold a stitch. The posterior sheath is not strong enough to serve as a definitive repair on its' own. I brought the midline together as best as I could and placed an absorbable mesh over the midline. I had considered some acellular porcine collagen, but the stuff we had was only 2X7 cm. The mesh's main purpose was to prevent evisceration should the fascial repair fail in the short term. The key words here are "in the short term" since it is inevitable he will get a hernia.
The skin edges were debrided and undermined inferiorly. A large sump drain was placed in either flank and some JP drains were placed anteriorly. The finished product:


He is undergoing an ORIF of his spinal fracture at this time. Time will tell how the wounds do. I'll keep you updated.
This is one of those cases that if I never see one again during my career it will be too soon. Be warned, some of the images are very disturbing.
20-ish restraint status unknown driver in a single vehicle collision. Questionable loss of consciousness. Impressive finding on physical exam (which I will reveal later). Some select views of his CT scans:

Air surrounding the right kidney and a questionable pneumoperitoneum:

Even more air. Here are some images from the CT of his lumbar spine:
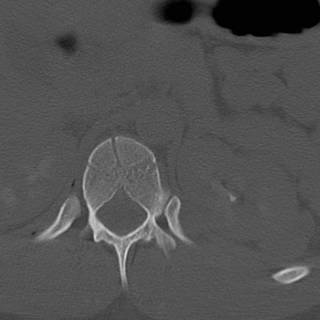

Appears to be a L1 compression fracture on the reconstruction.

Ouch!! So off we go to the OR for bilateral chest tubes (he had bilateral pneumothoracies on CT) exploratory laparotomy and reconstruction of his abdominal wall. The following images may not be suitable for all viewers:
[
]
[
]
[
]
[
]
[
]
[
]
[

[
]
[
]
[
]
[
]
[
]
[
OK YOU WERE WARNED!!!!
[
]
[
]
Here is how he presented to the ED. This photo was taken in the OR after application of a betadine scrub:
 From the left.
From the left.

And from the right. The most medial tissue seen in the left-sided incision is the posterior rectus sheath. Moving along:

Here are the right and left inferior portions of the rectus muscles. Remember this was done during the collision, probably by the seat belt. The superior portions had retracted upward.

The cecum is to the patient's right. Highlighted is a portion of denuded small bowel. Several other mesenteric tears were found in the last 21/2 feet of small bowel. The overlying bowel was intact and appeared to be perfused. This was confirmed by a Wood's lamp exam after injection of fluorescein. The segment pictured above was resected and an ileocolic anastomosis performed. Did a rather extensive lookaround. The duodenum was Kocherized and both kidneys were reflected medially. It was then time to put his abdominal wall back together.
The skin and subq fat were separated along the left flank posteriorly that I felt the tips of the 11th and 12th ribs. It extended to the posterior axiilary line on the right. The transversalis and oblique muscles had been divided on the left. I reapproximated them using their fascial layers to hold the suture. There was no good way to reapproximate the rectus since the muscle would not hold a stitch. The posterior sheath is not strong enough to serve as a definitive repair on its' own. I brought the midline together as best as I could and placed an absorbable mesh over the midline. I had considered some acellular porcine collagen, but the stuff we had was only 2X7 cm. The mesh's main purpose was to prevent evisceration should the fascial repair fail in the short term. The key words here are "in the short term" since it is inevitable he will get a hernia.
The skin edges were debrided and undermined inferiorly. A large sump drain was placed in either flank and some JP drains were placed anteriorly. The finished product:


He is undergoing an ORIF of his spinal fracture at this time. Time will tell how the wounds do. I'll keep you updated.
Labels: Tales from the Trauma Service
|Monday, January 03, 2005
Hope Springs Eternal....
From the Atlanta Journal-Constitution: Legislature to try again on tort reform.:
The sidebar of the article has details of a bill that has already been submitted for the 2005 session. Some high points:
Not Dr. Cole. |
From the Atlanta Journal-Constitution: Legislature to try again on tort reform.:
Doctors in white smocks, trial lawyers in power suits and medical malpractice victims in wheelchairs are expected to fill Capitol hallways during the upcoming Georgia General Assembly. Once again, they will wage a high-stakes, big-money lobbying campaign over caps on jury awards.......
.....But with Republicans now controlling both houses of the Legislature, coupled with the exit of a number of influential lawyer-legislators who opposed capping medical malpractice jury awards, the probability of tort reform seems higher than ever.
On both the national and state levels, few issues generate as much campaign cash and lobbying muscle as tort reform. It pits two well-financed interests against each other: trial lawyers and health care providers.
Doctors and hospitals continue to press the issue because, they say, swelling malpractice insurance premiums caused by soaring jury awards and legal settlements are driving doctors out of Georgia. Citizens groups and trial lawyers counter that limiting jury awards will do little to ease insurance rates; instead, they say, it will deny medical malpractice victims the right to be compensated justly for their injuries.
The sidebar of the article has details of a bill that has already been submitted for the 2005 session. Some high points:
Cap non-economic jury awards to victims at $250,000 to $750,000, depending on whether there are multiple defendants who are held liable.The hope is to prevent the multi-million "pain and suffering" awards that are out there, and allow for some predictability.
Prohibit non-economic damages from being awarded except in instances of "willful or wanton misconduct" to patients who become victims of a health care provider's malpractice within the first 24 hours after a visit to anI like this a great deal. Many patients in this situation fall under EMTALA, perhaps the most expensive unfunded federal mandate in existence. Physicians are forced to provide care in stressful situations to patients that may or may not have coverage, and in the case of trauma patients, are likely to sue someone anyway. The risk/reward calculation in this situation has forced many subspecialists to withdraw from emergency room coverage.
Prohibit lawyers from venue-shopping to get jury pools more favorable to plaintiffsI was not aware of such problems occurring in Georgia, Mississippi yes, but in Georgia?
Require juries to precisely apportion damage awards in multidefendant casesThe elimination of "joint and several liability". This would also help in keeping physicians available for coverage. Patient care could also be improved, since patients with complications or difficult conditions are often shunned because no one wants their name on a chart that is likely to end up in court.
Strengthen the standards and requirements for expert witnesses.At a legislative "meet and greet" a few weeks ago hosted by the local medical society one of the local legislators, heavily involved in environmental activism, was wringing her hands over how such "expert witness" legislation could hamper her pet causes. My pet cause is preventing stuff like this from happening. Via Overlawyered and the Allentown Morning Call: The county had no neurosurgeon, and the boy died
Robert Surrick of Chester County was angry over the death of a 17-year-old boy following a traffic accident.It's even happening here:
''He had head trauma,'' Surrick told me. ''They took him to Brandywine.'' The boy could not be treated at Brandywine Hospital in Coatesville because the trauma center had closed, so he was transferred to Crozier-Chester Medical Center in Delaware County.
''By the time he got there, he was dead. It was two hours from the time of the accident until they got him to Crozier,'' he said, noting it's crucial that neurosurgeons see head trauma patients within an hour.
''The last neurosurgeon in Chester County was Sam Lyness, a world-class neurosurgeon,'' Surrick said, but Lyness left Pennsylvania when his malpractice premiums reached $383,000. With no neurosurgeons, Brandywine shut down its trauma center in 2002.
The issue of capping jury awards sparks the most heated dispute. The Medical Association of Georgia says caps are essential to keep malpractice insurance premiums from rising to levels that force doctors to leave the state or retire early.Your young college student in Athens is in a car wreck or falls, who will be there to take care of them?
Dr. Geoffrey Cole, 48, a neurosurgeon in Athens, said he is giving up his practice to pursue a master's degree in business administration and work for HealthPlan Select, a hospital insurance company.
"Some might say I'm at the peak of a career," Cole said. "If the medical liability climate was more favorable, I'm sure I would have reached a different decision."
Not Dr. Cole. |







