Thursday, September 30, 2004
Nice profile in today's Atlanta Journal-Constitution of CNN's Dr. Sanjay Gupta: At CNN, the doctor is always IN
Somewhere, wherever unaired videotape goes to die, there's a rare artifact: a Sanjay Gupta goof.Dr. Gupta not only keeps up his busy schedule with CNN, he also practices at Emory University:
As TV bloopers go, this one was tiny. But you had to smile, if only at the irony, when CNN's unflappable Gupta misspoke recently while taping an "AccentHealth" segment.
"No good for Sanjay," somebody yelled after Gupta, 34, who had just nimbly negotiated "interstitial cystitis," flubbed an easy, nonmedical word. "It's supposed to be 'unsuccessfully.' He said 'successfully.' "
War and the outside world seemed far away on a recent Monday, when Gupta and two Emory residents spent about eight hours doing complex spinal operations at Grady. Geeky, black Buddy Holly-esque magnifying eyeglasses covered the TV doc's famous face, and nurses hovered over hundreds of exotic-looking instruments. Yet it felt almost calm amid the beeping machines and occasional murmured "Irrigation, please."Dr. Gupta was involved in a minor controversy during his coverage of the Iraq War when he performed surgery on an Iraqi civilian:
"There's always a sense of urgency, but not chaos," Gupta says. "I always tell my residents, 'It's OK to have butterflies. Just make sure they're flying in formation.' "
Gupta became part of the story temporarily when the neurosurgeon-less Devil Docs asked him to perform brain surgery on a gravely injured Iraqi child. Ultimately, Gupta operated on five seriously wounded people, leading some journalism observers to wonder if he'd blurred the lines."Journalism ethics specialist" no wonder the news is so screwed up.
"How does Gupta the reporter and Gupta the doctor reconcile his competing roles and competing obligations?" the Poynter Institute's journalism ethics specialist Bob Steele wrote at the time. "Does the Hippocratic oath duty always trump the journalistic responsibility to gather information and report stories?"
The criticism took Gupta somewhat aback, because he always knew who he was.
"I had a very clear moral compass out there," Gupta says. "You never stop being a doctor, and you never stop being a human being."
His biggest fan might be Jesus Vidana, a 26-year-old Marine Reserve sergeant so seriously wounded by a sniper's bullet in Baghdad that medics initially declared him dead. Gupta operated on him, and Vidana, now back home in Los Angeles, keeps in touch with the man he credits with saving his life.
Cross-posted at Galen's Log |
Tuesday, September 28, 2004
Go and check out Grand Rounds at Blogborgymi. It is one grand rounds that won't put you to sleep!
Even The Professor agrees! |
Teenaged male presents with three day h/o severe abdominal pain. Crampy in nature and it awoke him from sleep. Positive for nausea and vomiting. No BM since onset of pain. Admitted to the hospital by his pediatrician. WBC at that time was 12 with 90 neutrophils, no segs. His glucose is elevated. Abdominal film obtained:

His symptoms do not improve. A hemoglobin A1C is obtained and is 6.4. A sed rate today is 4. A CT scan of his abdomen and pelvis is obtained today:
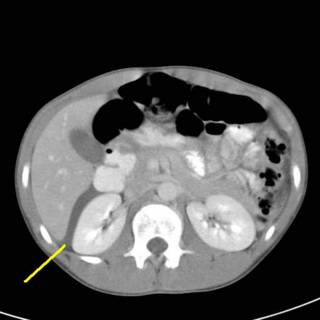
Fluid seen in Morrison's pouch. His pancreas is enlarged according to the radiologist.

Now we see some dilated small bowel loops and more fluid.
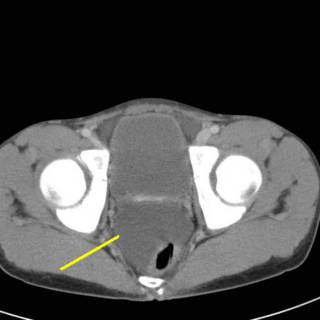
Fluid in the pelvis which has displaced his rectum.
I am asked to see this patient. He is very uncomfortable. His abdomen is distended with diffuse guarding. He is thin and muscular so that is not surprising. His bowel sounds are very faint. He really doesn't have any rebound. His urine is clear. His alkaline phosphatase, amylase, and lipase are all normal. This patient doesn't really add up to me. I obtain another CBC and while his WBC's are now 9, he has a left shift. I have mentioned the "sleep test" before, and I just could not imagine sleeping well tonight if I sat on this kid. Sometimes it is best to "operate first and ask questions later".
Let's take a look.....
WARNING! WARNING!!! The following images may be offensive!!!

O.K. YOU HAVE BEEN WARNED!!!

Here is what I found. The black line points to the cecum, the yellow line to the terminal ileum and the red line to what appears to be a Meckel's diverticulum.

Just to give you an idea of size. I wear 81/2 gloves.
I bathed it in warm saline, I stared at it hard and spoke lovingly to it. I had the CRNA give the patient an ampoule of fluorescein and did a Wood's lamp exam. The black area unsurprisingly did not light up. The amount of small bowel was about 2 feet. If any of the ischemic bowel had lit up at all I would have done a limited resection and come back for a second look in 24 hours. But given its' appearance, I did not think there was much to be gained from that.

Here is the ex vivo specimen. You can see the band that served as the axis of the volvulus. 35 percent of Meckel's diverticula (MD) present with obstruction.
MD is often called the "condition of twos". It is twice as common in males, contains two types of tissue (gastric and pancreatic), usually two inches long, occurs within two feet of the ileocecal valve, and occurs in 2 percent of the population. MD is often confused for appendicitis.
This is the first MD I have encountered, it was truly memorable. |
Sunday, September 26, 2004
Kevin strikes again with the New York Times take on acalculous biliary pain or biliary dyskinesia (BD). The concept of BD is that patients have pain similar to that of classical biliary colic due to stones, but have no gallstones on ultrasound. It is diagnosed with a CCK-HIDA scan which contracts the gallbladder. The cutoff is an EF of 35 percent. Oftentimes the patient will have a reproduction of their symptoms upon injection of the CCK.
I will often see these patients after a workup similar to that described in the story. I tell them that about 2/3 will get relief from the surgery. That looks to be a lowball figure based on the latest studies. Those that have some signs of chronic inflammation, such as adhesions, will stand a better chance of getting improvement. What is interesting is that the study Kevin cites, 85% of those with an EF> 35% had improvement. So line right up for your lap chole...
I will be the first to admit that BD fits the description of a "surgical nail". The whole concept of cholecystectomy for a non-calculous condition would be very hard to sell without the benefit of laparoscopy.
Cross-posted at Galen's Log |
Saturday, September 25, 2004
Hat tip to Kevin for linking to this Forbes story about a potential physician work stoppage in Maryland. I found this article in a Maryland paper: Threat of strike raises stakes in debate on insurance premiums
Surgeons in Washington County will begin turning away patients whose conditions are not life-threatening in hopes of forcing insurers to lower their malpractice premiums.Rates increasing by a third! Ouch!!!
The work stoppage is scheduled to begin Nov. 15 with a majority of the county's general surgeons, who handle a variety of procedures from appendectomies to vascular repairs.
But dozens of surgeons and physicians in other specialties are expected to announce soon that they also will begin turning down non-emergency work in November, said Dr. Karl P. Riggle, a spokesman for the Washington County Surgical Association.
The move could be the most drastic yet taken by medical doctors in Maryland, most of whom face a 33 percent increase in their insurance premiums. Doctors claim the rising rates are caused by large malpractice award payouts and threaten to drive them out of business, but their call for tort reform has been opposed by trial lawyers.
Don't think it can work? Think again. Just look at West Virginia:
a large group of northern panhandle surgical specialists stopped all their elective cases. Hospitals in the area, which were already struggling under inadequate reimbursement, began to suffer mounting losses in income. The hospital association’s involvement in the lobbying effort intensified dramatically.This brought national attention to the matter. And it got tort reform passed in West Virginia:
Critical portions of the tort reform bill include a $250,000 cap on noneconomic damages and a $500,000 cap on all damages for treatment of emergency conditions for patients who receive care at a designated trauma center. Joint liability has been eliminated, and each individual defendant bears liability equal to his or her percentage of fault. Collateral payments, which had not been allowed in court before, may now be presented. The “ostensible agency theory” of liability was abolished. Additionally, a committee was established to develop a patient injury compensation fund to provide for economic damages that exceed financial limits set in the bill.Will the physicians in Maryland do as well? It is an election year, you know.
And now, back to Star Wars Battlefront....
Cross-posted at Galen's Log |
Thursday, September 23, 2004
Poor Medical Treatment Kills Thousands in U.S., Says New Report on Health Care Quality
Requiring doctors and hospitals to report publicly on their performance and tying their pay to the results would dramatically reduce avoidable deaths and costs attributable to poor medical care, says a new report from an organization that works to improve health care quality.Well at least they aren't stating we actively kill people as the IOM did. The report, which may be found in PDF form here, uses indicators of preventative health measures (immunizations, cancer screenings) and some therapies (beta blockers) and reviews health plans compliance with those indicators. This is then extrapolated into statistics such as "avoidable deaths" (page 11) as well as "avoidable/non-fatal events" (page 12). To come up with these they took eight quality measures :Advising Smokers to Quit, Beta-Blocker Treatment After a Heart Attack, Breast Cancer Screening, Cervical Cancer Screening, Cholesterol Management - Control, Comprehensive Diabetes Care - HbA1c Control, Controlling High Blood Pressure and, Timeliness of Prenatal Care. Then :
Wild variations in medical care led to 79,000 avoidable deaths and $1.8 billion in additional medical costs last year, the private National Committee for Quality Assurance said in its annual report released Wednesday.
Using the data above as a baseline and comparing it to the 90th percentile care offered by the best health plans, we can calculate the expected avoidable mortality and morbidity for a number of the nation's most common, costly and deadly diseases if everyone received care through one of the top plans.So the study shows the expected mortality, which according to the summary is estimated to be between 42,000 and 79,000. The report provides no detail of how those figures were calculated. Certainly a range that large cannot reflect much reliability of the estimates. Anyway it is a far cry from "poor treatment kills thousands".
Another part of the report has to do with "pay for performance" using benchmarks such as this for indicators. So if you have the right percentage of your patients on beta blockers, control their cholesterol, and scold them enough about smoking you can buff your numbers and your paycheck will reflect that. Some programs already in place are described.
I wonder when they will start coming up with such detailed studies of surgical benchmarks? There are already some out there for such things as breast conservation versus mastectomy but certainly not as many as seen here.
Cross-posted at Galen's Log |
Monday, September 20, 2004
In the September 20 issue of Newsweek the recent interaction of President Clinton with the business end of an operating room is used to bring attention to the changing perceptions of surgery as a career: A New Style in the Operating Room
Under the lights of his operating room at New York Presbyterian Hospital, heart surgeon Dr. Craig Smith looks like a futurist, using high-tech robotic techniques on elderly patients once deemed too fragile for major surgery. Outside the OR, he's pure old school, with a deadpan wit and a schedule of 16-hour days. A college running back, he says he copes with stress by "keeping my emotions canned up and focusing on the job." To perform a "relatively routine" quadruple bypass on former president Bill Clinton last week, Smith postponed his 34th-wedding-anniversary vacation. He's just what Americans picture when they think of a surgeon: brilliant, stoic, workaholic and male.In fact, that cuts both ways. Sometimes you can be faced with a situation of a patient dies regardless. Under those circumstances one may be reluctant to offer the procedure. The match for surgery actually hit bottom in 2002 when of the 1039 positions offered, only 782 were filled by U.S. graduates and only 981 slots were filled overall. But the data also shows that roughly half of the family practice and internal medicine positions are filled by U.S. graduates. But there are more slots offered for IM and FP, and more family physicians and internists out there. The medical establishment looks to recent changes to try and stem the tide:
In the near future, surgeons like Smith may be the exception, not the rule. Since 1999 surgery has attracted about 5 percent of medical graduates—down dramatically from the 12 percent it pulled in the '80s and '90s, when the best and brightest students saw it as both intellectually enriching and, well, enriching. Surgical insurance premiums began to climb in the late '90s, making the field look a lot less lucrative. In some areas of the country, premiums have doubled or more since 2000, with surgeons paying well over $100,000 annually just to stay in business. Meanwhile, in an effort to boost enrollment and create a generation of doctors (particularly surgeons) who were more than technically proficient geeks, medical schools started recruiting a new kind of student—someone more laid back, with interests outside work. And they've succeeded: lifestyle-friendly specialties like radiology, orthopedics and dermatology are thriving. Anand Rughani, a third-year student at McGill, was toying with surgery but will probably choose neurology instead. Surgery "is so demanding," he says. "It can change your values. With lawsuits, you treat things fairly aggressively for fear of not doing something. Maybe surgery isn't the best thing for the patient, but that's what you end up having to do."
Medical schools are struggling mightily to bring students back to the OR with promises of a kinder, gentler professional future. New rules established last year dictate that medical residents can work a maximum of 80 hours a week—far fewer than the 120 hours traditionally demanded by surgery residencies—and courses in bedside manner are now mandatory in many curricula. The old guard isn't necessarily happy. "It's difficult to explain to my generation, who worked 120 hours a week, how people with two thirds as much training are going to get the same experience," Smith says. Duke University's surgery program was put on probation in June, partially for a citation related to lax enforcement of the 80-hour workweek.Such "reforms" will take years to bear fruit, if any is to be had. One problem that may rear its' ugly head in the near future is what to do if residents are not getting a sufficient number of cases. In order to sit for the boards a surgical resident must perform a certain number of cases over the five clinical years of their residency. If the amount of time spent in the hospital is reduced by 1/4 to 1/3, there can be problems obtaining the required experience.
Alternatives would include either reducing the number of cases required, eliminate the workhour limits, or prolong the length of the residency. The first option would not serve the surgeon or patient well, the second would not pass muster with the ACGME, and the last would take an already long residency and lengthen it further. That would do little to entice the "laid back" student with "interests outside of work" . The effects of this aren't likely to be seen for several years
As the boomers age, demand is likely to increase—just as today's young surgeons, accustomed to lighter schedules, start taking senior positions. Smith, at 55, toils as many hours as residents do. "If you like the work, it's tolerable," he says. But if you want your anniversary off, maybe you should go into neurology.Cross-posted at Galen's Log |
Sunday, September 19, 2004

Georgia 13 Marshall 3
Offense sputters along again but the defense held strong. Bob Pruett, head coach of Marshall put it thusly:
"They've got some good players. They've got to score more than 13 points to win a national championship."|
Wednesday, September 15, 2004
Ivan is on the way. Big Hsopital will decide today whether to cancel elective cases tomorrow and Friday. A local university has already cancelled classes. The power was out at the Acme Surgical Corp for a good part of the day after Frances. Looks like tomorrow is going to be a wet one...

|
Tuesday, September 14, 2004
Does Dr. Rangel have some sort of crystal ball? In his post concerning whole body CT scanning he signed off with this nugget of his rapier wit:
My advice to the wealthy and paranoid; Change over to magnetic resonance whole-body scanning. It may be more harmful to your wallet but it has no proven cancer risk and is just as useless as a screening exam. Have fun!Well, well from Medscape today comes: Whole-Body Screening MRI: What You and Your Patients Should Know
In recent years, there has been considerable interest in direct patient referral for imaging studies to screen the whole body for disease detection. In general, the majority of the facilities that have been performing whole-body screening have done it with new, fast, multidetector computed tomography (CT) systems. Speed of data acquisition, in the order of a few minutes for the entire body, has made it a compelling method of investigation. There are some limitations and concerns with CT, described briefly below, but the major focus of this Clinical Update is whole-body screening with magnetic resonance imaging (MRI). Within the last few months, this has become a feasible approach, the most important advances being a dramatic increase in data acquisition speed concurrent with maintenance of high image quality.The article then goes on to describe the recent technological advances which have made the use of MRI as a screening tool feasible. Some hurdles remain, however:
Optimal investigation for many diseases requires using dynamic administration of gadolinium chelate (a type of intravenously administered contrast agent that is in routine use in MRI), and because MRI can image only about 40 cm in vertical length of a person in 1 data acquisition (essentially 1 of 4 major regions: head and neck, chest, abdomen, or pelvis), this would involve too many separate injections of contrast (eg, separate injections for the liver, heart, and breast [in women])......A nice compare and contrast can be found on this page. In summary:
Presently a confounding variable exists with protocols for whole-body screening. It is widely recognized that several organ systems are currently imaged by MRI with an extremely high level of diagnostic accuracy and reproducible image quality (eg, liver, pancreas, kidneys, brain, spine, musculoskeletal system, gynecologic organs, and major blood vessels) that exceeds the abilities of CT.[4-11] However, despite recent technical advances, described at the beginning of this Clinical Update, the diagnostic accuracy is not high for prostate, coronary vessels, colon, or breast, secondary to such factors as decreased sensitivity, decreased specificity, or inconsistent display of small and/or moving structures.
1.Ionizing radiation is bad if you don't need it. No such problem with MRI
2. Non-contrasted CT is fast and avoids potential reaction problems, but they are lousy as screening studies, not such a problem with MRI.
3. The use of contrast improves sensitivity, but problems abound. Gadolinium is fairly safe.
4. The rate of injection is slower with MRI which causes less side effects
But as of now, CT is far cheaper than MRI. But I'm sure it will be only a matter of time before MRI scanners open up at a strip mall near you.
Cross-posted at Galen's Log |
Another urban trauma center about to bite the dust: King/Drew Trauma Unit Faces Closure:
The Los Angeles County Board of Supervisors on Monday unexpectedly moved to shut down the trauma unit at Martin Luther King Jr./Drew Medical Center, immediately drawing the ire of physicians, politicians and community activists.The trauma unit treated 2150 patients last year, in one of the most violent sections of Los Angeles:
The only public hospital serving a large swath of South Los Angeles, King/Drew treats more trauma patients than any other hospital in the region except County-USC Medical Center.
The proposed trauma closure, expected to take effect in about 90 days, amounts to a last-ditch scramble to save a foundering hospital that repeatedly has been cited by regulators for harming patients and in some cases contributing to their deaths.
County officials said they would make every effort to persuade other hospitals to open trauma centers. But health experts said the loss of King/Drew could further jeopardize a beleaguered system that has lost about 10 trauma units in the last two decades. The county now has 13, including King/Drew.King-Drew Medical Center has been under a cloud of scandal for several months:Watts Symbol of Hope Becomes Center of Conflict
Just two of the county's trauma centers are within 11 miles of King/Drew: Harbor-UCLA and St. Francis medical centers.
King/Drew serves one of the most violent areas of the county, with the highest rate of homicides.
"Closing down a [trauma unit] within a couple miles of the most violent parts of the city? South Los Angeles? Compton? Lynwood?" asked Sal La Barbera, homicide supervisor in the Los Angeles Police Department's Southeast Division station, which covers Watts. "This will definitely have an impact on how many lives are saved . Harbor [UCLA] is an extra 10 or 15 minutes."
King Hospital and its affiliated medical school, the Charles R. Drew University of Medicine and Science, have been rocked by accusations of needless deaths, racial tension, poorly trained medical students and incompetent nurses and tens of millions of dollars in malpractice settlements.As the man selling the Ginsu knives says, but wait, there's more:
King/Drew consistently ranks at the bottom of American teaching hospitals. A report in January by federal health officials said that at least five of the hospital's patients died needlessly last year, and the county authorities are investigating accusations that hospital officials ordered nurses to lie about the abysmal state of things.
''The hospital is run like a tribal fiefdom, and it's appalling,'' said Connie Rice, a civil rights lawyer here who is African-American. ''You can't ask questions because it's a black institution. If you ask questions, they scream racism. But it's not a question of race, it's a question of competence.''....
According to the January federal audit, three people died last year in ward 4B, where the nurses did not know how the heart monitoring machines worked.
A man who was suffering from gangrene of the intestines was brought to the emergency room last March and was found 18 hours later lying in his vomit, having received no medical care. He later died. Another man suffering from gangrene was neglected for the better part of a day and died, the audit said......
A national accreditation board last year rescinded the private medical school's authority to train surgeons and radiologists. The county has temporarily severed the hospital's relationship with the medical school, because of the quality of education.
A woman with respiratory failure and ovarian cancer received the wrong dosage of an antibiotic on Feb. 28; did not receive an ordered dose of a blood thinner on March 1; and was given only three of 12 ordered doses of respiratory drugs from Feb. 28 to March 2.In the past whenever the hospital was criticized the response, as pt forth by Ms. Rice above, was to play the race card, and in the past have played it well:
A stroke patient had to wait nearly five hours for a drug to help prevent heart attacks and recurrent stroke. At one point, pharmacists wouldn't fill the order because a doctor had spelled the drug's name wrong. Later an inspector watched as two pharmacists within half an hour picked up the pill bag and looked at it but did not approve its use.
In the case of a tuberculosis patient, an inspector found a missing dose of intravenous antibiotics on a pharmacy counter more than two hours after it had been ordered, with a sticker that read "missing dose." The inspector noted errors in three of six medications given to the patient.
A paraplegic with a pressure sore and bone infection was not given a laxative suppository that had been ordered and reordered by a physician over at least five days.
The hospital's supporters are not sitting still. A rally co-sponsored by the Congress of Racial Equality in late January showed just how deep the racial tensions are. Representative Maxine Waters, Democrat of California, warned county officials that if the neonatal unit was closed, ''we will be on top of your desk.''Reread that last quote carefully gentle reader. Seems to imply that the deaths are no big deal, the big deal is that they are getting the attention of the press and casting the hospital in an unfavorable light.
In a telephone interview, Ms. Waters elaborated. ''What we're saying is we're going to watch you,'' she said. ''The county only reacts when the spotlight is on them. They're not going to close that hospital. They can't close that hospital. They need to supervise it, and shuffling a few people around isn't going to do it.''
Dr. Ernest Smith, an instructor in the Drew University department of internal medicine who is African-American, is outspoken in his criticism of the county health department, which he sees as unfairly laying blame at the feet of the black administration.
''When things go wrong, why do they point the fingers at administrators and not the master down there at 313 North Figueroa Street,'' Dr. Smith said, referring to white officials at the county health department. ''Maybe the place would operate better if we received our fair share of money.''
Health department officials say, however, that King/Drew receives more money per patient from the county than any other hospital in the system. ''The quality of the administrators isn't there that a hospital needs,'' said John Wallace, spokesman for the county health department. ''It's been allowed to go on for years.''
Yvonne Brathwaite Burke, a black county supervisor whose district includes the hospital, admits there are some problems at King/Drew. But she said the problems had been blown out of proportion. ''It's not a matter that you go there and you die,'' she said, ''it's that the press picks up on every little mistake.''
According to the LA Times the trauma unit is not being closed because it is bad, but in an effort to relieve "pressure" on the rest of the hospital:
The closure of the trauma unit, officials said, does not stem from failings in the unit, which has long been a source of great pride and prestige to the community. At one point, the U.S. military trained surgeons in the unit because it so closely simulated wartime medicine
Rather, the proposed closure is intended to relieve pressure on the rest of the hospital. Running a trauma unit is costly because the patients are so sick, many are uninsured and the hospital is required to have a host of specialist doctors on standby 24 hours a day to respond immediately when an emergency arises.
The fact that hospitals and their boards are highly politicized is nothing new. The image of a hospital, urban or rural as a nepotistic jobs program, or as Ms. Rice puts it a "tribal fiefdom" is also nothing new. The problem arises when the administration insulates themselves from criticism by using the methods applied here, and because of that insulation people die and a community suffers.
Cross-posted at Galen's Log |
Monday, September 13, 2004
Tales from the OR continues....50-ish year old woman with a history of diverticular perforation in the past which required a 3-stage procedure (drainage/diversion, resection, and finally colostomy takedown) to resolve about 3 years ago. Had symptoms c/w ulcerative colitis and underwent uneventful colostomy and biopsy. About 8 hours post-procedure she began to c/o chest and neck pain. Went to the ED and obtained the following CXR:

The yellow lines point to air in unusual places. I wasn't entirely convinced that the air along the right diaphragm was intraperitoneal as you could not see the line of the right hemidiaphragm all the way to the midline. Obtained a CT scan:

Which shows both intraperitoneal and retroperitoneal air.

The amount of air is such that the kidney is outlined.

There is a hernia at the old stoma site. The air in the mesentery appears here. The preop diagnosis was a colonic perforation due to the colonoscopy. The treatment for this is exploration and primary repair. Primary repair is possible due to the prepared colon after a colonoscopy.
Upon entering the abdomen there was not the usual audible rush of air that comes with entry into the peritoneum. An extensive adhesiolysis followed and I was fortunate not to create an enterotomy. Given the preponderance of the air on the right side my efforts were concentrated there. There was a good deal of air within the wall of the colon and mesentery. No spillage, gross perforation, or colonic ischemia was seen. The colon was defatted extensively. This was approached gingerly since if a hole was discovered, the question could come up was it there, or did I create it? After all this I had three options: blind resection, close up and go home, or provocative testing. Given the late hour the tests I could perform were limited. Here's what I did.
Bowel clamps were placed on the terminal ileum and distal transverse colon. The colon was cannulated with a 16-gauge angiocath and about 400cc of air was insufflated. This achieved a distention similar to that of colonoscopy. The colon was submerged under saline and observed for bubbles. None seen. Given the possibility of a perforation into the mesentery that air may not reveal, I then instilled about 250cc of methylene blue solution. No blue anywhere. Did the same thing to the left side of the colon, no spillage. Gave it several looks during closure, still no blue. There was not only frustration that no perforation was found, but a concern that I was missing something.
There is a level of comfort in the practice of medicine and surgery that can be roughly described as the "sleep of the just". I think you know what I mean. Cases like this do little to help my sleep. But I thought that a blind resection was too radical, that any clinically significant perforation would have been identified. I closed and went to bed.
She is doing well. Postop CXR shows resolution of the free air. |

Georgia 20 South Carolina 16
I missed the first quarter because I was attending a meeting. Kind of glad I did. The Dogs were able to find a way to win regardless. This can be viewed two ways, one is that championship teams need to overcome obstacles such as this to build themselves. The other is that teams bound for greatness avoid such problems. I agree with the former, and hope it is true.
|
Thursday, September 09, 2004
Heinz Kerry: Opponents Of Health Care Plan Are 'Idiots'
Teresa Heinz Kerry says "only an idiot" would fail to support her husband's health care plan.So join me, Galen, Mr. McBride, Dr. Smith,Dr. Centor, and others in the Parade of Idiots!!!!
But Heinz Kerry, the wife of Democratic presidential candidate John Kerry, told the (Lancaster) Intelligencer Journal that "of course, there are idiots.".....
If Kerry is elected, Heinz Kerry predicts that opponents of his health care plan will be voted out of office. She says, "Only an idiot wouldn't like this."
Sign up today!!
Via Drudge
Cross-posted at Galen's Log |
Tuesday, September 07, 2004
There are topics which get a great deal of play in the medical blogosphere which have little to do with my surgical practice. Retainer medicine is one and the other is the debate over pharmaceutical issues. I have read with great delight the posts by Galen and Mr. McBride in response to Dr. Centor's call to ban direct to consumer pharmaceutical advertising as well as physician detailing. There isn't much DTC advertising for surgical products, for many reasons. One is the yuck factor. Imagine an ad for an intestinal stapler:
"When the time comes for your colectomy...make sure your surgeon uses the Ajax Mark II linear stapler...The Mark II has the lowest rate of fecal leak of any stapler on the market"That would go over real well during the dinner hour!
Another is the fact that surgeons sometimes have limited options. Many companies have "saturation contracts' with hospitals. That is, if a device is used, say 80 percent of the time, the manufacturer gives the hospital a discount. Also if many different products by a particular manufacturer are used, a discount is given. The big surgical stapler makers, Ethicon and U.S. Surgical, frequently use such agreements. I remember when the hospital where I trained had a trial of U.S. Surgical suture. They had been using the staplers for years and had been offered a deal if they would buy their suture as well. The trial did not go well for two reasons, one is that surgeons have been trained for years with Ethicon suture and old habits are hard to break, and secondly the USSC suture was awful.
There is also the mechanism for getting new devices into you local OR. One way is a company approaches the purchasing manager of the hospital or OR. This is the approach many companies use when they have a similar device that they claim can beat a competitor on price. If successful they can have their products available for trial, and if enough physicians get behind it the device can be stocked. Another way is a physician is approached by a rep or visits a booth during a meeting. The manufacturer provides some of the devices (i.e. the Ajax stapler) to the physician gratis and if the surgeon likes them, they ask the purchasing manager for it and the request works its way through the bureaucracy and may or may not be approved. For big-ticket items (retractor systems, ultrasound machines, and the like) you usually have to wait for the yearly capital budget process.
But some surgical firms are getting into the act as well. Over the weekend I saw an advertisement for Stryker Ceramics pitching their products for joint replacement, using Jack Nicklaus as a pitchman. I mean if John Elway can shill for Prevacid, why not? So I'm sure some orthopedic surgeon is being pressured to use their product because a patient saw it on TV. SoonZimmer will be forced to respond. I believe things are not exactly as described above for total joint implants, since the patient's insurance is billed directly by the manufacturer rather than the manufacturer billing the hospital which then bills the patient. So DTC advertisement in this situation can influence decision-making. Glad to see we are catching up with the drug makers.
Cross-posted at Galen's Log |
The single-payer crusader, in response to my earlier post sent me a link about waiting times and how they "not always a bad thing": Tackling Excessive Waiting Times for Elective Surgery: A Comparison of Policies in Twelve OECD Countries
It was educational to find out that 38 percent of patients in the United Kingdom had a wait time of over four months for elective surgery. The authors think that wait lists help maintain the "optimum rate of surgery". If no waiting list existed, their reasoning goes, there would be an excess of surgical capacity, which is expensive. There are some charts which give the ideal rate of surgery as when the marginal cost equals the marginal benefit. There are also mechanisms both from a supply side (increase capacity or start some production-based incentives) and a demand side (raising requirements to be on the list.) The increased use of outpatient surgery is advocated, but with caution:
In the last twenty years there has been a steady growth in the share of surgery carried out by daysurgery in many countries, thanks mainly to technological and medical innovations, such as less invasive surgery and better anaesthetics. Day-surgery is beneficial because it reduces the unit cost of treatment, which is driven by the length of stay. For a given endowment of beds, the availability of less invasive surgery can increase the volume of treatments performed and free up hospital beds. However, if the increase in day-surgery utilisation is accompanied by a contemporaneous reduction in the number of hospitals beds (as in most OECD countries), then the net impact on activity may be lessened. Moreover, less invasive and safer treatments raise the net benefits for the patient, making the procedures more desirable. That is likely to lead an increase in demand, especially for groups such as the very elderly, for whom there would otherwise be counter-indications for invasive surgery. The final effect on waiting times is then indeterminate.Another problem arises since most of the minimally-invasive outpatient surgery procedures require the use of expensive equipment. The expense of this may trump any LOS gains realized.
The authors also advocate wait lists as a means to stabilize surgical demand over time. That is, every system should have an "emergency buffer" such as the extra unused OR or the extra CRNA around. Not very efficient but very useful when the ruptured aortic aneurysm shows up. The wait list is used as a "ready reserve" of patients which can fill up a slow day in the OR.
The darker side of wait-lists can be found in this article:
Risk of emergency admission while awaiting elective cholecystectomy
Waiting lists are a common tool for managing access to elective surgery. However, little evidence is available on the health impact of delaying surgery for various conditions. Other than mortality, adverse events experienced by patients while on a waiting list have not been systematically examined. Without these data, appropriate access time for surgery must be determined on the basis of expert opinion.
When treatment is delayed, the condition of a patient on a surgical waiting list may deteriorate and require urgent medical attention. In this case, emergency admission for the awaited procedure may be regarded as an adverse effect of waiting. Also, routine operating room activity may be seriously disrupted by unexpected nonelective admissions of patients on waiting lists.
In patients with biliary colic caused by cholelithiasis, extended treatment delays may increase the probability that the patient will be admitted for delayed cholecystectomy as an emergency case. Emergency admission may be associated with more frequent or more severe attacks of biliary colic or other biliary complications such as acute cholecystitis, obstructive jaundice, cholangitis or pancreatitis. However, little is known about the relationship between time spent on a waiting list and the risk of emergency admission in these patients....
The median length of stay on the list was 6 weeks. However, there was considerable variation in individual waiting times. The probability of undergoing elective surgery increased rapidly from 25% within 3 weeks of the last clinic visit to 50% at 6 weeks and 75% at 10 weeks, and then gradually reached a plateau. Although 90% of patients underwent surgery by 17 weeks, the remaining 10% waited another 1 to 3 weeks (total 1852 weeks) for their operation.....
the weekly emergency admission rate increased from 0.8 to 5.7 per 100 patients from the first 4 weeks to the interval of 40-52 weeks. When adjusted for sex, age, enrolment period and surgeon volume, the emergency admission rate was more than 1.5 times higher after 20 weeks, 2 times higher after 28 weeks and 7 times higher after 40 weeks relative to the first 4 weeks of waiting-list time.
And it appears that need or chronology played little role in determining the waitlists of some surgeons:
Surgeons with a low volume of cholecystectomies (less than 20 per year) operated on the majority of patients with extended delays. In general, low-volume surgeons had a primary interest in surgical oncology. This may explain the order in which their patients accessed cholecystectomy during the waiting period.No joke.
If wait-lists are an unavoidable, even desirable, effect of single-payer systems, will the population at large in America buy into it? I doubt it.
Cross-posted at Galen's Log |
Monday, September 06, 2004
Watching the press conference by President Clinton's surgery/cardiology team:
Sounds like a LIMA to the LAD and marginal, a RIMA to the circumflex and a SVG to the right coronary. This should serve him well given the improved patency of arterial grafts.
Was done on-pump due to "anatomic" considerations according to Dr. Smith.
Crossclamp time 73 minutes.
The surgeon looks irritated by some of the questions. Many questions along the lines of "when can he get out and campaign for Kerry"
"How much did this cost?" Please....
Questions about the delay, reason given was to allow Plavix to clear.
Questions about the neurocognitive effects of cardiopulmonary bypass. Surgeon quotes 30 percent incidence of defects, many which resolve over a year.
Press conference now over.
Cross-posted at Galen's Log |
Sunday, September 05, 2004
While removed somewhat from hurricane Frances at this time accoring to the 3 day projected path, what will become tropical depression Frances will come just to the west of the Parker abode.

While the wind shouldn't be too bad there could be up to 10 inches of rain. It is due to arrive Tuesday morning, just in time for my office day. |

Georgia 48 Georgia Southern 28
Ahh, college football now in full swing. The Bulldogs looked like they had left their defense in the locker room during the first half but came back to lead at one time 41-14. Spectacular performance by freshman running back Danny Ware. Even better games were the overtime contests between Clemson and Wake Forest as well as Louisiana State and Oregon State. |
Thursday, September 02, 2004
What if you went to the prom and you had to wait too long for a dance, or some punch, or the line to the bathroom was winding around the gym floor? Is it a lack of suitable partners, not enough refreshments, or broken plumbing? Is it because your prom committee underestimated demand or spent the ticket money foolishly? Or is it because the prom guests are drinking too much punch and taking too much time in the john? Or, to step away from the wilted corsages and ruffled-front tuxedos, is the rationing that goes hand-in-hand with a single-payer system due to a lack of resources or too much utilization by patients or physicians? While the conventional wisdom states that both are to blame, this article places the emphasis on the latter:We can cut waiting lists by cutting into fewer patients:
When the talk turns to waiting lists -- as it does often in political circles these days -- there is an assumption that waits for surgery are caused by inadequate resources.
If we only had more surgeons, more operating rooms and more money, the thinking goes, we could clear up this pesky problem.
If only it were so simple....
A team of researchers from the University of Alberta and the University of Calgary showed that almost half of carotid endarterectomies (an operation to clear blocked arteries in the neck) are of questionable value, and that 10 per cent of these surgeries are entirely inappropriate and probably dangerous to patients.
A second study, conducted by Health Canada, found that the mastectomy rate varies dramatically from one province to the next, which likely means that hundreds, maybe even thousands, of women are having their breasts removed unnecessarily.
The carotid study published in the August 31 edition of the Canadian Medical Association Journal indicates, according to the criteria they used, that overall 52 percent of carotid endarterectomes (CEA) were done appropriately, ten percent were inappropriate, and the remainder were of "uncertain indication". I don't have time today to dissect that paper further, as I am on call. I cannot find a citation of the mastectomy article at this time.
Moving along:
These are but two examples, but there are many more. The vast majority of tonsillectomies were dubious; lower back surgery, once the rage, provided little pain relief in the long term; medically unjustified hysterectomies, gall bladder removals, cesarean sections and cataract operations are legion. More recently, some solid studies have shown that surgery for arthritic knees is of no value, and that "active surveillance" of some cancerous tumours is more effective than surgically removing them.When Worlds Collide: EBM versus consumer demand. Much like the demand for pricier medications described here there are some patients who will press for surgery. The accusations put forth above seem to tar with a pretty wide brush the medical profession. How do they define a "medically unjustified" cholecystecomy or hysterectomy? I hope the solid tumor under "active surveillance" is prostate cancer and not something else.
I have patients all the time come in with conditions which are not amenable to surgery at all or have not reached the point to where surgery is helpful. Two ways to avoid trouble: don't talk patients into having an operation and don't let them talk you into giving them one. When thing go badly (as they can do) you won't have much of a leg to stand on. I have cancelled patients in the holding area when they began to question their desire for surgery. I have had others see other surgeons when I passed, some did well, others did not. "The customer is always right" does not apply to medicine and may be dangerous when used as justification for surgery, but now I'm just being paternalistic.
One of the criticisms of a single-payer system is the demand for services will rise when the out-of-pocket cost is reduced to zero. The article above seems to place more of the blame on the physician rather than the patient. I am sure both are a little to blame.
Cross-posted at Galen's Log |
Having voted for Zell Miller multiple times in the past and being a big fan of his, I was eagerly awaiting his speech last night.
Oh my. I was not disappointed. He did an excellent job of slapping Chris Matthews around after the speech was over.
And according to rumor, that was a "toned down" version.
The text here
Video here. |
Wednesday, September 01, 2004
Three hits from this weeks New England Journal of Medicine.
The first:Tamoxifen with or without Breast Irradiation in Women 50 Years of Age or Older with Early Breast Cancer
Background We determined the effect of breast irradiation plus tamoxifen on disease-free survival and local relapse in women 50 years of age or older who had T1 or T2 node-negative breast cancer.
Methods Between December 1992 and June 2000, 769 women with early breast cancer (tumor diameter, 5 cm or less) were randomly assigned to receive breast irradiation plus tamoxifen (386 women) or tamoxifen alone (383 women). The median follow-up was 5.6 years.
Results The rate of local relapse at five years was 7.7 percent in the tamoxifen group and 0.6 percent in the group given tamoxifen plus irradiation (hazard ratio, 8.3; 95 percent confidence interval, 3.3 to 21.2; P<0.001), p="0.004)." p="0.049),"
So the disease-free survival rate after five years was 84 percent in the Tamoxifen only group compared to 91 percent in the Tamoxifen+XRT group. Local recurrence was 7.7 percent in the Tamoxifen only group and 0.6 percent in the Tamoxifen+XRT group after five years. These rose to 17.6 and 3.5 percent,respectfully, after eight years. There was a slight increase in ipsilateral axillary recurrence in the Tamoxifen-only group. As has been shown repeatedly, there was no difference as to overall survival.
And now the second:Lumpectomy plus Tamoxifen with or without Irradiation in Women 70 Years of Age or Older with Early Breast Cancer
Background In women 70 years of age or older who have early breast cancer, it is unclear whether lumpectomy plus tamoxifen is as effective as lumpectomy followed by tamoxifen plus radiation therapy.|
Methods Between July 1994 and February 1999, we randomly assigned 636 women who were 70 years of age or older and who had clinical stage I (T1N0M0 according to the tumornodemetastasis classification), estrogen-receptorpositive breast carcinoma treated by lumpectomy to receive tamoxifen plus radiation therapy (317 women) or tamoxifen alone (319 women). Primary end points were the time to local or regional recurrence, the frequency of mastectomy for recurrence, breast-cancerspecific survival, the time to distant metastasis, and overall survival.
Results The only significant difference between the two groups was in the rate of local or regional recurrence at five years (1 percent in the group given tamoxifen plus irradiation and 4 percent in the group given tamoxifen alone, P<0.001). p="0.94)."
Again, radiation rules the day with a three percent reduction (96% to 99%) of local recurrence after Tamoxifen+XRT. While the XRT group had more adverse effects such as retraction or hyperpigmentation when compared to the Tamoxifen only group, most of those resolved within 1 year and all within four years. Both studies had about 700 patients. One problem I had with the second study was this statement:All women underwent lumpectomy (i.e., partial mastectomy or a wide local excision) with a clear margin, defined by the absence of tumor on the inked pathological margins. Axillary-node dissection was allowed but was discouraged
So some of these women may have been understaged. Now for some tidbits from the editorial:Breast Radiotherapy after Lumpectomy - No Longer Always Necessary:Does this absolute difference in the rate of local recurrence of 3 percent matter clinically, when weighed against the cost of the use of additional resources and treatment-related adverse effects? An overview of 40 trials in this field has confirmed that local radiotherapy is associated with an increase in deaths from cardiac and other causes, which nullifies a long-term reduction in deaths from breast cancer Modern radiotherapy techniques, including three-dimensional treatment planning and intensity-modulated radiotherapy, with cardiac shielding, can minimize the risk of cardiac irradiation in most patients Some side effects persist, and the CALGB investigators reported an increased incidence of breast pain, fibrosis, breast edema, and poor cosmetic results in the group that received radiotherapy. In addition, breast radiotherapy is resource-intensive and time-consuming for the patient and may decrease the quality of life There is, of course, the counterargument that not having radiotherapy may increase a woman's anxiety about the possibility of recurrence and could require more frequent follow-up. On balance, nevertheless, there are clear advantages in identifying subgroups in a large population of elderly women who do not require radiotherapy after lumpectomy and tamoxifen......
Against this background, what course should we recommend to older women with small, hormone-receptorpositive breast tumors who have undergone lumpectomy? The Canadian trial indicates that women under the age of 70 years should still receive radiotherapy in addition to tamoxifen. This is frustrating advice, because although it is clear that the majority of women treated with lumpectomy and tamoxifen alone would not have a relapse, we still cannot confidently predict which women will be in the majority. We are entering an era in which the use of molecular markers, gene-expression profiles, and other molecular prognostic indicators is being investigated as a means of individualizing adjuvant medical therapies,15 and there is no reason why the same approach should not be applied to radiotherapy. Future trials of radiotherapy should be required to include tissue biopsy for prospective molecular analyses and informed consent for this type of research.
As our understanding of breast cancer has evolved, so has our ability to treat it in the most effective, minimally invasive way possible. We have gone from the morbid Halstead radical mastectomy to local resections and perioperative radiation. Clear margins are becoming recognized as a more important risk factor than absolute tumor size. We are witnessing the evolution of the axillary dissection from a requirement to an operation of historical interest.
So the take-home is: for a small, selected group of patients (older than 70, small tumors, receptor positive) then benefit of radiation may not outweigh the morbidity, given the less aggressive course of breast cancer in the older population. This may prove to be a hard sell, given the fact that 899 of the 1572 patients eligible to enroll in the first trial declined.
Cross-posted at Galen's Log






