Monday, May 09, 2005
The 80-hour Workweek and Operative Experience......
From the Journal of the American College of Surgeons:Impact of Work-Hour Restrictions on Residents’ Operative Volume on a Subspecialty Surgical Service
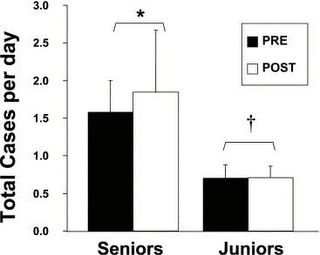
Data from the 2002 and 2003 academic years were compared. The senior residents were PGY 3&4 and the juniors were PGY 1&2. Procedures were broken down by class as well:
A slight but insignificant increase of senior level cases after the implementation of the rules. Now the operative experience, by class, of senior residents:
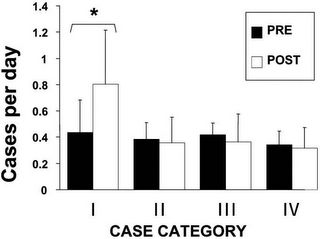
The vast majority of the increase comes from a large increase of the "minor cases". The p value for that increase was 0.03. Now for the junior residents:
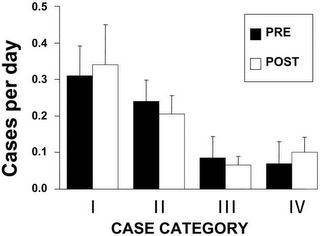
Again some difference but nothing statistically signifigant. This program has done much to comply with the hour limits:
From the Journal of the American College of Surgeons:Impact of Work-Hour Restrictions on Residents’ Operative Volume on a Subspecialty Surgical Service
Background
Whether the 80 hours per week limit on surgical residents’ work hours has reduced the number or variety of cases performed by residents is unknown.
Study design
We quantified residents’ operative experience, by case category, on a pediatric surgical service. The number of senior and junior residents’ cases were compared between residents from the year before (n = 47) and after (n = 44) the 80-hour limit. Residents also completed a questionnaire about their operative and educational experience. As an additional dimension of the educational experience, resident participation in clinic was assessed. Student’s t-test was used.
Results
Total number of cases performed either by senior (before, 1.58 ± 0.42 versus after, 1.84 ± 0.82 cases/day) or junior (before, 0.70 ± 0.21 versus after, 0.71 ± 0.15) residents has not changed (p = NS). Senior residents’ vascular access and endoscopy rate increased; other categories remained stable. Residents’ perception of their experience was unchanged. But residents’ participation in outpatient clinic was significantly decreased (before, 66.0% ± 14.7% versus after, 17.0% ± 19.9% of clinics covered, p < 0.005).
Conclusions
The 80-hour limit has had minimal impact on residents’ operative experience, in case number and variety, and residents’ perceptions of their educational experience. Residents’ reduction in duty hours may have been achieved at the expense of outpatient clinic experiences.
Data from the 2002 and 2003 academic years were compared. The senior residents were PGY 3&4 and the juniors were PGY 1&2. Procedures were broken down by class as well:
Category I included all endoscopic procedures and vascular access procedures. Category II included simple, open surgical procedures. Major open procedures—both abdominal and thoracic—were placed into Category III. Category IV included all minimally invasive procedures.The residents filled out a questionnaire asking how certain aspects of the training program had changed due to the implementation of the 80 hour workweek. Items included educational quality of weekly conferences, quality of teaching received from surgical attendings, quality of teaching received from pediatric surgery fellows, amount of time available for reading, number of cases they had participated in, degree permitted to participate in cases, variety of cases exposed to during the month, rate the amount of independent decision making entrusted to them, degree to which residents had been involved in patient management, and overall, qualitative assessment of the educational value of rotation. No statistically significant difference was seen between the "pre-limit" and "post-limit" results. The differences were most apparent in the staffing of clinic and the case mix of the senior residents.
A slight but insignificant increase of senior level cases after the implementation of the rules. Now the operative experience, by class, of senior residents:
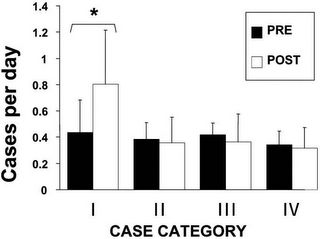
The vast majority of the increase comes from a large increase of the "minor cases". The p value for that increase was 0.03. Now for the junior residents:
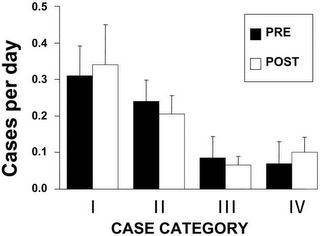
Again some difference but nothing statistically signifigant. This program has done much to comply with the hour limits:
Before the ACGME mandate, residents in our program regularly worked well beyond 80 hours per week, a documented characteristic of many surgical residency programs. The dramatic changes necessitated by the 80-hour limit were unprecedented in our residency program. To comply with the requirements, after July 1, 2003, duty hours were closely monitored, and junior residents were required to leave the hospital at 10:00 am on the morning postcall. Even with this change, compliance with the 80-hour limit was not always achieved; and within a few months, the postcall residents had to be relieved of duty after 8:00 am. With this system, compliance with the 80-hour limit was achieved. We were surprised to find that the actual number of residents’ operative cases did not decrease. It may be that residents—to avoid a loss of operative experience—consciously made extra efforts to scrub into cases during their allotted time in the hospital, after the 80-hour limit took effect. Although Sawyer and colleagues have demonstrated that resident participation in surgery decreases with increasing frequency of call (every other night, versus every third or fourth night), frequency of call was unchanged in our study. Both before and after the 80-hour week, residents took call every third night.I wish I could take off at 8 AM on a post call day. The impact of case-mix and senior level resident participation can be significant as programs adapt:
Another point to be mentioned is that restructuring of the service took place in the last few months of the study, with removal of the senior from the service, leaving only junior residents under the supervision of the pediatric surgical fellows. This restructuring was a direct result of compliance with ACGME regulations. In the future, it is certainly conceivable that this type of restructuring of resident rotations may result in an overall decrease in number of cases performed by a senior-level resident on some subspecialty services. Data describing the operative experience of general surgery residents on surgical subspecialties such as pediatric surgery (for which the ACGME requires residents to log a specified number of cases) are very scarce.This is a phenomenon that is widespread. This study re-enforces the concept that upper level residents are more affected by hour limits that the junior ones:
We found that seniors performed significantly more vascular access and endoscopic cases after the 80-hour week was in effect. The explanation for this is not immediately apparent, but several previous studies have indicated that senior residents may be affected by work-hour limits more than juniors. In New York, 35% of residents reported that duties had been shifted from junior to senior residents to comply with work-hour limits. Our finding may represent this type of phenomenon, as cases in Category I are likely to be less highly sought after by upper-level residents than cases in the other categories. Our data suggest that a minor shifting of junior responsibilities to seniors may have occurred.So senior residents are performing cases usually reserved for the junior residents, because the junior residents all leave the hospital at 8 AM 1 out of every 3 days. So will the skills of these residents in two to three years be equal to the senior level residents that are rotating today? This would be a very interesting study to repeat in a few years. |






